What is Hydrocephalus?

Hydrocephalus is a condition caused by the accumulation of cerebrospinal fluid in the brain. The brain is located in the cranial cavity. It is a closed space with constant volume. Yet, the brain does not occupy the entire space in the cranium. It is surrounded by cerebrospinal fluid (CSF). CSF is continuously produced in the brain by the choroid plexus. It fills brain ventricles and subarachnoid space. There are four ventricles in the brain connected to subarachnoid space.
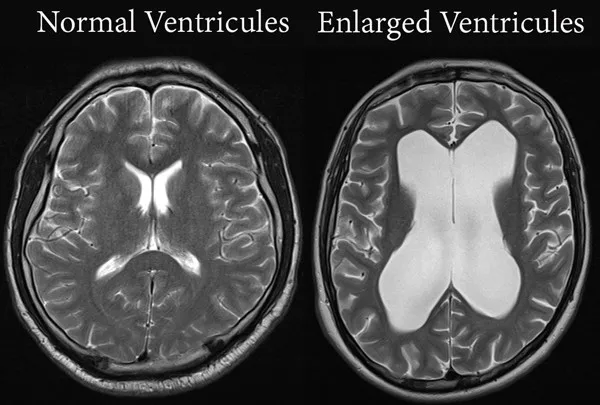
Enlarged Ventricles and CSF Dynamics
CSF passes from ventricles to subarachnoid space, and then it is reabsorbed into blood circulation by the system of arachnoid granulations or villi. Cerebro-spinal fluid is constantly produced and reabsorbed. Daily CSF production is about 600 ml, and the total volume of cerebrospinal fluid in the central nervous system is approximately 150 ml. Therefore, CSF is renewed 4-5 times every day. CSF production is pressure independent – meaning that no matter what the pressure inside the brain, the amount of newly formed CSF is constant.
On the other hand, absorption of the CSF is pressure-dependent. The higher the pressure in the subarachnoid space, the higher the absorption rate. This peculiar mechanism maintains normal pressure inside the cranial cavity and optimizes brain functions.
Fluid on the Brain: How does Hydrocephalus develop?
Hydrocephalus is the disturbance of this balance when the fluid accumulates in the brain. Usually, the cause is either a blockage of the flow or insufficient absorption. Fluid builds up in the brain, raising the pressure inside of the head.
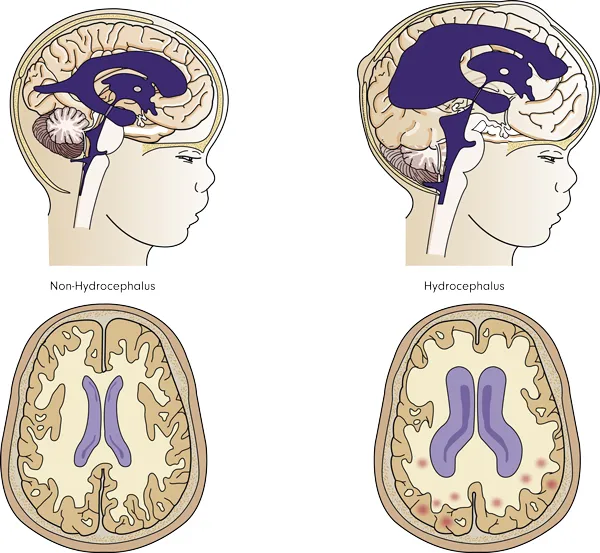
Since the cranium is a closed space, even a small amount of extra fluid causes a significant increase in pressure. Elevated pressure in the brain is an extremely dangerous condition and should be treated promptly. There is one exceptional form of hydrocephalus when the pressure does not rise. It is called normal pressure hydrocephalus (NPH), and it is seen only in elderly patients.
What Causes Hydrocephalus?
Hydrocephalus is caused either by increased production of CSF, blockage of flow, or decreased absorption. Here are a few conditions associated with hydrocephalus.
Obstruction or narrowing in the ventricular system. Aqueductal stenosis, foramen Monro stenosis, colloid cyst, intraventricular arachnoid cysts, tumors, and bleeding into ventricles are examples of this type. In these cases, CSF cannot flow freely, causing hydrocephalus. The mechanism is quite similar to gallbladder or kidney outflow obstruction by stones.
Obstruction within subarachnoid space. Meningitis, subarachnoid hemorrhage, and cancer spreading into subarachnoid space are well-known examples. Hydrocephalus is frequently seen after subarachnoid hemorrhage due to aneurysms. This form of hydrocephalus is caused by both obstruction of CSF flow in the subarachnoid space and blockage of absorption by arachnoid granulations.
Normal pressure hydrocephalus. It is a specific form of disease seen only in elderly patients. In this condition, the pressure is not high. Rather, the brain cannot tolerate normal pressure, and hydrocephalus develops.
Hydrocephalus Symptoms in Adults and Babies
Symptoms of hydrocephalus are drastically different in babies and adults. In babies, the skull is capable of growing, and therefore, fluid accumulation does not significantly increase the pressure. Rather, it leads to the increased size of the head. In older children and adults, hydrocephalus cannot distort the head. Rather, it increases intracranial pressure, compromising brain functions.
Headache is the most common symptom of increased intracranial pressure. This pressure stretches the brain covers – especially the dura mater. Dura mater has many pain receptors and is very sensitive to pressure. The brain itself does not feel the pain.

Other symptoms include nausea, vomiting, and altered consciousness. Vision disturbances are very common in hydrocephalus. Blurred vision due to optic nerve compromise is a very common finding. Eye movements are also frequently compromised. Parinaud symptom or upward gaze palsy is very common in hydrocephalus. Also, the VI cranial nerve can be compromised by increased intracranial pressure and cause an inability to look to the side.
The severity of symptoms depends on the pressure and onset time. Acute hydrocephalus is poorly tolerated because the brain cannot switch on compensatory mechanisms. It is usually a life-threatening condition and should be treated promptly. Chronic hydrocephalus may not be symptomatic for a long time.
Normal Pressure Hydrocephalus (NPH) and Its Triad
Normal-pressure hydrocephalus (NPH) is different from other forms. It is always chronic and characteristically has three main symptoms – dementia, gait disturbance, and urinary incontinence. Any elderly patient with dementia should have a brain scan to rule out the possibility of NPH since it is the only treatable form of dementia.
Hydrocephalus Diagnosis

Clinical examination with a careful history of the disease is the first step for establishing the diagnosis. In babies, increased head size is easily detected, and diagnosis can be made right away.
Adult patients can be unconscious and, therefore, may not be able to provide history. Careful neurologic examination, especially looking for visual disturbances, helps to suspect hydrocephalus.
Radiological examination is of paramount importance in diagnosing hydrocephalus. Brain CT and MRI are preferred choices. MRI is superior to CT in demonstrating the inner structure of the brain. In any case, ventricular dilatation is clearly appreciated on brain scans and is a hallmark of the disease.
How is hydrocephalus treated?
Surgery is the only permanent treatment option for hydrocephalus. In rare cases, the underlying reason is transient, and therefore, temporary measurements such as external ventricular drainage (EVD) might be helpful until the underlying condition is spontaneously eliminated. For example, bleeding into the ventricular system with acute hydrocephalus can be managed with EVD. The catheter is placed into the ventricular system with the purpose of draining CSF outside. The pressure is relieved, and thus, the patient’s condition improves. The blood clots are eventually eliminated, the CSF flow pass is re-established, and the catheter is removed.
The best way to manage hydrocephalus is to eliminate the underlying cause. For example, if there is an obstruction of the CSF pathways, eliminating the cause will cure the hydrocephalus as well. Tumor, blood clot, and cyst removal are examples of this treatment option.
However, in the vast majority of cases, the underlying cause cannot be eliminated, and hydrocephalus must be treated itself. There are two types of surgery – shunting and ventriculostomy. CSF diversion or shunting is a procedure in which the surgeon places a device called a shunt to redirect the fluid from the brain to another part of the body for absorption. Most commonly, the CSF is shunted to the abdominal cavity – so-called ventriculoperitoneal shunting. Usually, a shunt has three parts: ventricular catheter, valve, and peritoneal catheter. Ventricular catheter is placed into brain ventricles through a small hole in the cranium. The peritoneal catheter is placed right under the skin from head to belly and then placed into the abdominal cavity. Both catheters are connected with a valve which allows drainage of fluid when the pressure is high.
Endoscopic third ventriculostomy (ETV) is a procedure in which an artificial window is made to allow the CSF to bypass the blockage. A very thin endoscope is placed into the ventricle through a small hole in the head. The endoscope is then advanced into the third ventricle, and then a window is created on the floor of the ventricle. This opening allows CSF to flow from the third ventricle into subarachnoid space directly.
Both shunting and ETV are effective procedures to treat hydrocephalus. The main handicap of shunting is the implantation of a foreign device, which has to stay for the rest of the life. The shunt may get infected or have a mechanical failure. ETV, on the other hand, is an elegant and simple procedure, yet it is most effective when hydrocephalus is due to a blockage of fluid flow.