One increasingly recognized but still underdiagnosed condition is jugular vein compression caused by a tortuous carotid artery. This occurs when your carotid artery – the major blood vessel that carries blood to your brain – becomes abnormally curved or twisted and presses against the neighboring jugular vein, which is responsible for draining blood back out of your brain. When this drainage pathway becomes blocked, it can cause a wide range of frustrating symptoms.
In this guide, we’ll explain what causes this type of jugular vein compression, how it’s diagnosed, and what treatment options are available to help you find relief.
Understanding the Anatomy
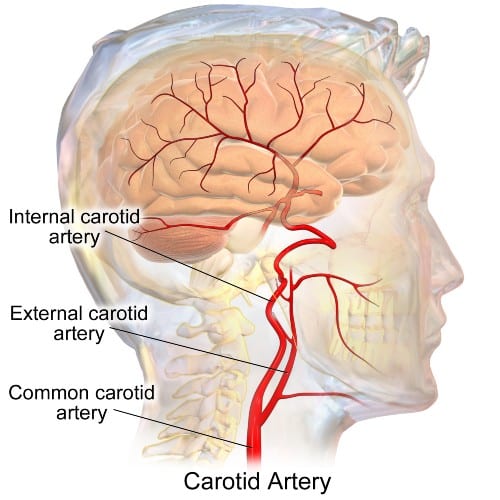
To understand how your carotid artery can compress your jugular vein, it helps to know how these blood vessels are arranged in the neck.
The internal carotid artery and internal jugular vein travel together inside a protective sleeve of tissue called the carotid sheath. Think of this sheath as a narrow tunnel running from the base of your skull down through your neck, containing these two vital blood vessels plus the vagus nerve. 1
Here’s the key point: while the artery has thick, muscular walls, and high internal pressure the jugular vein has much thinner, more flexible walls and much less internal pressure. This design allows the vein to expand and contract with changes in blood flow, but it also makes the vein vulnerable to being squeezed by nearby structures. When the carotid artery becomes twisted or curved, it can press the jugular vein against the walls of the carotid sheath or against the bones of your spine, partially blocking the vein.
Approximately 750 milliliters of blood flows through the brain every minute, and this blood needs to drain back to your heart. The internal jugular veins are the primary drainage pathways. When these veins are compressed, blood has difficulty leaving your brain, creating a backup of pressure—much like what happens when you partially block a drain.
What Is Carotid Artery Tortuosity?
A tortuous carotid artery is one that has become abnormally curved, twisted, or kinked instead of following a relatively straight path. Doctors classify these abnormalities into three main types: 2
Type 1 – Tortuosity: The artery elongates and curves into a “C,” “U,” or “S” shape. This is the most common form.
Type 2 – Coiling: The vessel forms a loop or spiral, resembling a coiled spring.
Type 3 – Kinking: The artery makes a sharp bend at an angle less than 90 degrees—like a garden hose that’s been bent too sharply.
You might be surprised to learn that carotid artery tortuosity is actually quite common—studies suggest it occurs in 18-35% of the general population. 3 However, not everyone with a tortuous carotid artery will develop jugular vein compression or symptoms. Whether compression occurs depends on the degree of tortuosity, the exact position of the artery, and individual anatomical variations.
Who Is at Risk?
Several factors increase the likelihood of developing a tortuous carotid artery:
Age: This is the strongest risk factor. As we age, our blood vessels naturally lose some of their elasticity and can elongate or twist. Studies show the risk increases significantly after age 60, with particularly high rates after age 78. 4
Long-standing high blood pressure: Years of elevated blood pressure can cause the artery walls to weaken and the vessel to elongate. Interestingly, patients who take blood pressure medications appear to have some protection against developing tortuosity—another good reason to manage your blood pressure.
Elevated body weight: Research shows that for every 1 kg/m² increase in BMI, the risk of carotid tortuosity increases by about 1.6 times. 5
Connective tissue disorders: Patients with conditions like Ehlers-Danlos syndrome or Marfan syndrome have higher rates of blood vessel abnormalities, including carotid tortuosity. 6
Symptoms of Carotid-Induced Jugular Vein Compression
When the carotid artery compresses the jugular vein, it impairs blood drainage from your brain. This can cause a range of symptoms that often overlap with other conditions—which is why many patients go years without a correct diagnosis. 7
Common symptoms include:
- Chronic headaches: Often described as a pressure-like sensation, particularly in the temples. These headaches may worsen when lying down or bending over—positions that further impair venous drainage.
- Tinnitus: Ringing, buzzing, or pulsating sounds in the ears. Many patients describe a “whooshing” sound that matches their heartbeat (pulsatile tinnitus).
- Visual disturbances: Blurred vision, visual field changes, or a feeling of pressure behind the eyes. Some patients report that their vision seems worse at certain times of day.
- Sleep problems: Difficulty falling asleep or staying asleep, often related to discomfort from headaches and tinnitus.
- Cognitive difficulties: “Brain fog,” difficulty concentrating, or memory problems that patients often find difficult to describe to their doctors.
- Neck discomfort: Stiffness or aching in the neck, sometimes with a sensation of fullness.
Important: Because these symptoms are nonspecific, patients are often initially diagnosed with other conditions such as migraines, anxiety, depression, ear problems, or even told their symptoms are psychosomatic. If you’ve been struggling with these symptoms and haven’t found an explanation, it may be worth asking your doctor about jugular vein compression.
How Is This Condition Diagnosed?
Diagnosing carotid-induced jugular vein compression requires imaging studies that can visualize both the blood vessels and their relationship to each other. Several tests may be used:
Ultrasound
Doppler ultrasound of the neck is often the first test performed. It’s non-invasive, widely available, and can measure blood flow through the jugular veins. Studies suggest that ultrasound may actually be more sensitive than MRI for detecting jugular vein stenosis. 8 If the ultrasound shows reduced flow or narrowing in the jugular vein, additional imaging is typically recommended.
CT Venography (CTV)
This specialized CT scan uses contrast dye to create detailed images of your veins. CTV is excellent for showing the exact location and cause of jugular vein compression. Three-dimensional reconstructions can clearly demonstrate how a tortuous carotid artery is pressing against the jugular vein. CTV is particularly valuable because it also shows the bony structures of your neck, helping to rule out compression from other sources.
MR Venography (MRV)

Magnetic resonance venography provides similar information to CTV but without radiation exposure, making it preferable for younger patients or those who may need repeated imaging. MRV can also show changes in brain tissue that might result from chronic venous congestion.
Catheter Venography with Pressure Measurements
In some cases, your doctor may recommend a more detailed study where a thin catheter is threaded into your jugular vein to directly measure the pressure difference across the narrowed area. This test can help determine whether the compression is severe enough to warrant treatment. A pressure gradient of 5.44 cmH₂O or higher across the stenosis is generally considered significant. 9
Treatment Options
Treatment for carotid-induced jugular vein compression depends on your symptoms, the severity of the compression, and the results of pressure measurements. Options range from conservative management to interventional procedures.
Conservative Management
For patients with mild symptoms or those whose pressure measurements don’t meet the threshold for intervention, medical management may help reduce symptoms:
- Medications to reduce intracranial pressure
- Blood-thinning or circulation-improving medications
- Management of underlying conditions (controlling blood pressure, addressing atherosclerosis)
- Symptomatic treatment for tinnitus, headaches, and sleep difficulties
Limitations: Conservative treatment manages symptoms but does not address the underlying compression. Some patients experience partial improvement, but symptoms often persist or return.
Jugular Vein Stenting
For patients with significant compression and elevated pressure gradients, jugular vein stenting may be recommended. This minimally invasive procedure involves placing a small metal mesh tube (stent) inside the compressed portion of the jugular vein to hold it open.
Studies have shown promising results with this approach. In one series, after stenting, headache resolved in 93% of patients, visual problems improved in 83%, and tinnitus resolved in 91%. 9

Important consideration: Stenting for carotid-induced compression is more complex than stenting for other causes of jugular compression (like styloid process compression). There is concern that placing a stent next to a tortuous carotid artery could potentially affect the carotid bulb—a structure involved in blood pressure regulation. Your doctor will carefully weigh the risks and benefits based on your specific situation.
Surgical decompression
Surgery provides the most definitive treatment for arterio-venous conflict. It is reserved for severe cases resistant to conservative treatment. During the procedure the surgeon separates the artery from the vein. The mobilized artery is moved away from the vein and affixed to nearby soft tissue. This way the physical contact between the artery and vein is eliminated. Compared to stenting this option has several advantages. First there is no need for stent – so no foreign material is inserted into the body. Therefore, there is no need for legthy anticoagulation therapy employed after stenting. Second arterial repositioning allows the vein to regain its normal shape and position.
What to Expect During Treatment
If you undergo jugular vein stenting:
- The procedure: Stenting is typically performed under local anesthesia or conscious sedation. A catheter is inserted through a vein in your groin and guided to the jugular vein, where the stent is deployed. The procedure usually takes 1-2 hours.
- Recovery: Most patients go home the same day or the following day. You’ll likely need to take blood-thinning medications for a period after the procedure to prevent clot formation in the stent.
- Results: Many patients notice improvement in their symptoms within the first few days to weeks. Follow-up imaging is typically performed to ensure the stent remains open and functioning properly.
- Follow-up: Regular monitoring with ultrasound or CT venography helps ensure long-term success.
Addressing Common Patient Concerns
How is this different from Eagle Syndrome?
Eagle Syndrome involves compression of blood vessels or nerves by an elongated styloid process (a bony projection from the skull) or calcified ligament. Carotid-induced jugular compression involves a different mechanism—the artery itself is compressing the vein due to tortuosity. However, both conditions can cause similar symptoms related to impaired venous drainage. Some patients may have both issues simultaneously.
Can this condition be cured?
While we cannot straighten a tortuous carotid artery, we can often relieve the jugular vein compression through stenting. Many patients experience significant, lasting improvement in their symptoms. However, because this is a relatively newly recognized condition, long-term outcome data is still being collected.
Is the compression on both sides?
Carotid-induced compression can be unilateral (one side) or bilateral (both sides). Case reports have documented patients with bilateral compression. If both sides are affected, treatment may need to address both, though this is typically done in a staged fashion.
Why wasn’t this found sooner?
Carotid-induced jugular vein compression is still an emerging area of medical knowledge. Many physicians are not yet familiar with this condition, and standard imaging may not specifically look for it. Additionally, the symptoms overlap with many other conditions, leading to misdiagnosis. As awareness grows, more patients are being correctly identified and treated.
What if I don’t get treated?
The natural course of untreated carotid-induced jugular compression is not fully understood. Some patients may have stable symptoms, while others may experience gradual worsening. Chronic impairment of venous drainage has been associated with changes in brain white matter on imaging, though the long-term significance of these findings is still being studied.
Conclusion
If you’ve been struggling with chronic headaches, tinnitus, visual problems, or cognitive difficulties without finding an explanation, jugular vein compression caused by a tortuous carotid artery may be worth investigating. While this condition is not yet widely recognized, awareness is growing, and effective treatments are available.
The key points to remember:
– A tortuous carotid artery can compress the adjacent jugular vein, impairing blood drainage from the brain
– Risk factors include age, long-standing high blood pressure, elevated body weight, and connective tissue disorders
– Symptoms include headaches, tinnitus, visual disturbances, sleep problems, and cognitive difficulties
– Diagnosis requires specialized imaging such as ultrasound, CT venography, or MR venography
– Treatment options include conservative management and jugular vein stenting
If you suspect you may have this condition, seek evaluation from a physician experienced in cerebral venous disorders. With proper diagnosis and treatment, relief is achievable.
Related: Jugular Vein Compression Treatment
Jugular vein compression can occur from multiple causes, including the styloid process (Eagle Syndrome) and the C1 vertebra. If your compression involves bony structures rather than a tortuous carotid artery, surgical approaches such as styloidectomy or C1 transverse process resection may be appropriate. Please see our comprehensive guide: Jugular Vein Compression Treatment for more information on these conditions.
Learn More About Jugular Vein Compression:
Jugular Vein Compression: A Detailed Review
Jugular Vein Compression: Treatment Options Explained
References
- Anatomy, Head and Neck: Carotid Sheath. StatPearls Publishing; 2023[↩]
- Tortuous Carotid Arteries and Their Clinical Implications: A Report of Two Cases. Cureus. 2023;15(3):e36953[↩]
- Han HC. Twisted blood vessels: symptoms, etiology and biomechanical mechanisms. J Vasc Res. 2012;49(3):185-97[↩]
- Age and duration of hypertension are associated with carotid artery tortuosity. Front Neurol. 2024;15:1307984[↩]
- Extracranial Internal Carotid Artery Tortuosity and Body Mass Index. Front Neurol. 2017;8:508[↩]
- Carotid Artery Tortuosity Is Associated with Connective Tissue Diseases. AJNR Am J Neuroradiol. 2019;40(10):1738-1743[↩]
- Li M, Su C, Fan C, Chan CC, Bai C, Meng R. Internal jugular vein stenosis induced by tortuous internal carotid artery compression: two case reports and literature review. J Int Med Res. 2019;47(8):3926-3933[↩]
- Laukontaus SJ, Pekkola J, Numminen J. Magnetic resonance imaging of internal jugular veins in multiple sclerosis: interobserver agreement and comparison with doppler ultrasound examination. Ann Vasc Surg. 2017;42:84-92[↩]
- Zhou D, Meng R, Zhang X, et al. Intracranial hypertension induced by internal jugular vein stenosis can be resolved by stenting. Eur J Neurol. 2018;25(2):365-e13[↩][↩]
