What is the failed back syndrome?

Failed back syndrome is a condition when back surgery does not provide the expected benefit to the patient. There are several failed back syndrome scenarios
- The surgery did not provide relief at all, and the patient’s symptoms continued as before the surgery
- There was an initial improvement period (“honeymoon period”), after which symptoms returned
- The symptoms worsened after surgery
What are the reasons that lead to failed back syndrome?
There are many different reasons that cause failed back syndrome.
Misdiagnosis
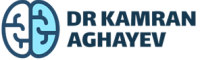
The patient’s condition may not be due to lumbar degenerative disease. For example, piriformis syndrome is a compression neuropathy of the sciatic nerve at the buttock level. The symptoms of this syndrome are pain, numbness, and weakness – very similar to lumbar disc herniation.
Therefore, misdiagnosis may lead to unnecessary low back surgery and obviously will not improve the patient’s condition. Another common condition frequently misdiagnosed as degenerative lumbar disease is sacro-ileitis. This condition is due to either degenerative or autoimmune inflammation of the joint between the sacrum and ileum. It causes pain in the lower back and is very often underdiagnosed or misdiagnosed as degenerative lumbar disease.

If the patient’s symptoms did not change at all after surgery, there is a strong indication that the true cause was not identified.
Failed back after lumbar disc herniation surgery
In cases of lumbar disc herniation, the symptoms may recur sometime after surgery. Lumbar discectomy is very effective in treating radiculopathy. This procedure involves removing the herniated part and compressing the nerve root. The surgeon then removes part of the degenerated nucleus pulposus. However, some of the degenerated nucleus material is left in place. Therefore, the remaining nucleus pulposus material may re-herniate through the existing annulus window and cause symptoms. Approximately 8% of disc herniations recur after the initial surgery.
Another common scenario is persistent low back pain following lumbar discectomy surgery. This syndrome is due to continuous pain originating from the degenerated disc responsible for herniation. Surgery effectively eliminates nerve root compression yet cannot cure disc degeneration itself. Thus, lumbar disc surgery cannot provide relief for low back pain originating from the damaged disc itself. Patients should be well aware of this important fact. Failure to properly educate patients before surgery may result in patient dissatisfaction.
Failed back after laminectomy
Historically, failed back syndrome was initially called post-laminectomy syndrome. Therefore, these two conditions are sometimes synonyms. Yet post-laminectomy syndrome is now considered as one of many forms of failed back.
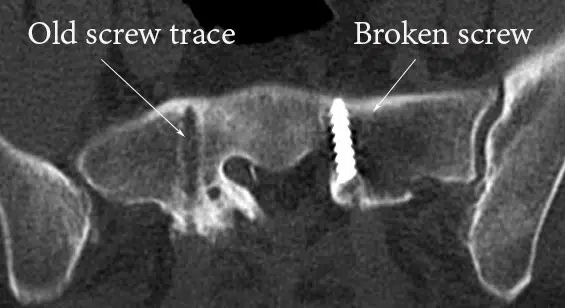
Laminectomy is a commonly performed procedure for spinal stenosis. Laminectomy is also used to surgically access the spinal cord for tumors, syringomyelia, and vascular and congenital malformations. It can be performed at any spinal level, but cervical and lumbar segments are the most frequent locations. Usually, it is performed for treating spinal stenosis. The surgeon removes the lamina (posterior portions of vertebral bones) to enlarge the spinal canal. The ligaments holding the lamina together are removed as well. These ligaments prevent excessive forward bending. Laminectomy is very effective in relieving the pressure from the spinal cord and nerves, yet it has several handicaps.
The spine loses back support after laminectomy. Therefore, kyphosis (bending the spine forward) is a very common condition following laminectomy. The greater the number of removed lamina, the higher the likelihood of kyphosis. This form of deformity shifts spine load to the front and causes positive sagittal balance. With time, it may progress further and cause significant deformity.
Intervertebral disc degeneration – the underlying cause of stenosis, is not affected by laminectomy. The stenosis goes on narrowing intervertebral foramina – nerve exits from the spine. This condition is called foraminal stenosis.
Lumbar fusion failure
A very common reason for failed back syndrome after spinal fusion surgery is the lack of bone fusion. There is a lot of misconception about fusion, and this article aims to clarify this topic in detail. Lumbar fusion and instrumentation are very commonly confused and interchangeably used terms.
Instrumentation, or more commonly hardware placement – is a procedure performed by the surgeon. The surgeon places cages, screws, bone grafts, or other means in order to stabilize a segment of the spine. The goal of this procedure is to achieve fusion sometime after surgery.
Fusion is a biological process by which two adjacent bones fuse together and become one solid bone. Bone healing after fracture is an example of fusion. Fusion has to take place following the surgery. The usual time period for fusion after lumbar instrumentation is approximately 6-12 months. If fusion fails to develop properly, the condition is called “failed fusion,” “non-union,” “pseudo-fusion,” or “pseudo-arthrosis.”
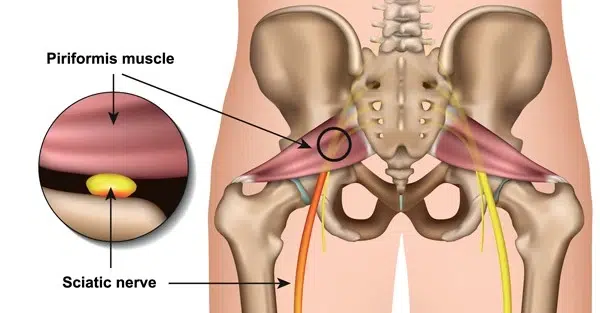
Non-union has two possible presentations – hardware failure or bone loosening. The spine is a mobile structure and moves a lot during daily activities. If fusion fails to develop at the instrumented level, this segment remains slightly mobile. The movement of this segment is restricted by hardware. In this case, the spine is literally fighting against the rigid hardware. There are two possible outcomes of this conflict – hardware failure and bone failure.
Hardware failure
Any metal has a fatigue lifetime, meaning that there are a number of times when it can be bent. With constant stress from the mobile spine, metal failure takes place and results in hardware breaks. The picture below belongs to a patient who had lumbar hardware placement. No fusion developed, and one of the screws broke inside the bone. A surgeon removed most of the hardware but could not retrieve the broken part.
Bone failure

In this scenario, constant movement from the body causes bone loss around the screws. Typically, this condition is best appreciated on a CT scan. The loose bone around bone screws creates a typical “halo” image on the scan and is very specific for this condition. With bone loss around the screws, the entire hardware becomes loose and may pull out from the bone.
Adjacent level degeneration
This condition is frequently encountered following the fusion procedure. Since fusion freezes a segment of the spine, disc joints in immediate proximity have to compensate for restricted overall motion. As a result, the neighbor joints become more loaded and degenerate faster. In this scenario, the patient improves after fusion surgery and may even become totally pain-free. But several years later, adjacent degeneration may cause the recurrence of symptoms.
To prevent adjacent-level degeneration, surgeons usually employ non-fusion techniques. Motion preservation is essential in keeping the spine’s physiology. Using artificial disc prosthesis instead of fusion significantly lowers the possibility of adjacent-level degeneration and repetitive surgery.
What are the symptoms of failed back syndrome?

The main symptom of the failed back syndrome is back pain. If there is ongoing radiculopathy, leg pain may accompany back pain as well. The pain is worsened by physical activity. Sometimes, patients may “feel” hardware in their back.
The pain is usually chronic and significantly affects a person’s quality of life. Depression and other psychological problems may develop in severe cases. In some cases, with ongoing nerve compression, pain radiates down the leg. Numbness, tingling, and weakness in the legs are also frequent symptoms. Sometimes, patients might need assistance with daily activities.
Diagnosing the failed back syndrome
Diagnosis of failed back syndrome is like assembling a puzzle. Every piece has to be placed correctly to make a correct picture.
Clinical examination is an essential step in the diagnosis of a failed back. Whether the patient benefited from initial surgery or not, did he/she had a “honeymoon” period, or did symptoms worsened after surgery is very important to suspect ongoing problems.
Radiological examination, including X-ray, CT, and MRI, helps to pinpoint the problem. Patients may have problems with spine coronal and sagittal balance, adjacent level degeneration, broken hardware, non-union, and herniation recurrence. These conditions are usually well-identified in imaging studies.
In some cases, electromyography (EMG) and nerve conduction studies can help with differential diagnosis. These studies are especially helpful for identifying radiculopathy and distinguishing it from peripheral nerve entrapment.
How is the failed back syndrome treated?
Correct diagnosis of the underlying problem is the key to success. In many cases, highly experienced specialists are required to find the reason and correct it.
Revision surgery is frequently performed for the failed back syndrome. The type and extent of surgery depend on the underlying problem.
The two most common scenarios are recurrent disc herniation and failed fusion. In either case, treatment usually consists of fusion.
Instrumentation with abundant, high-quality grafting is an essential step for obtaining robust fusion. However, revision surgery is more technically challenging than initial. Scar tissue formed around the spine and nerves significantly impedes surgical manipulation. Therefore, the rate of complications is higher in revision surgery. Therefore, this type of surgery should be performed by highly experienced neurosurgeons.