What is the pituitary adenoma?
A pituitary adenoma is a benign brain tumor arising from the pituitary gland.
Where is the pituitary gland located, and what are its functions?
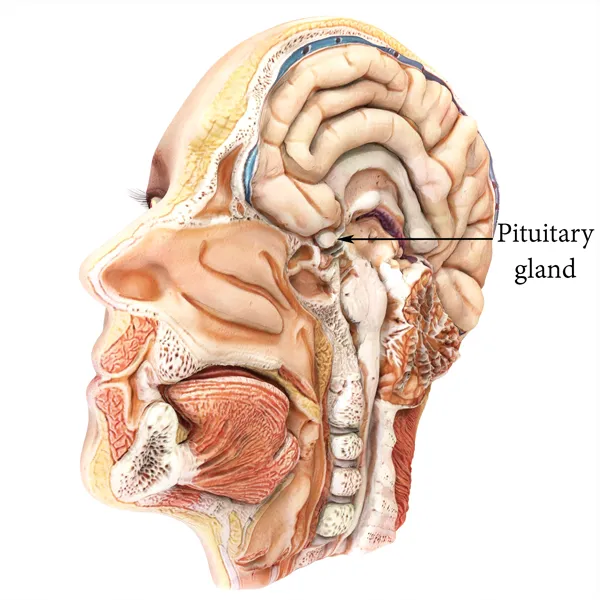
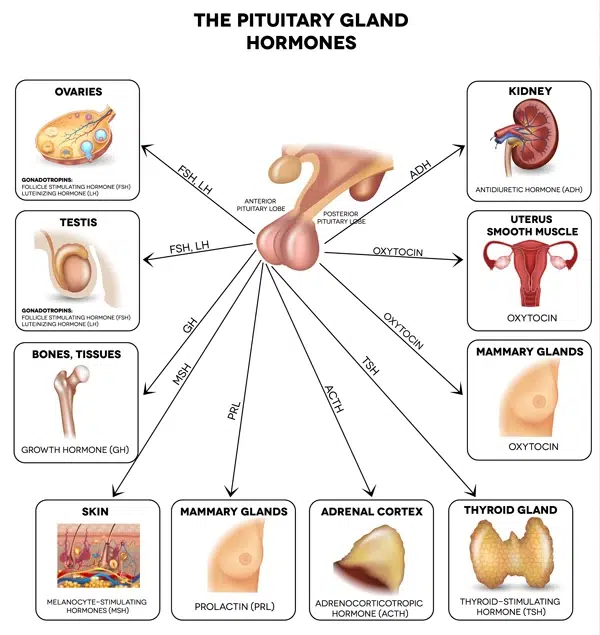
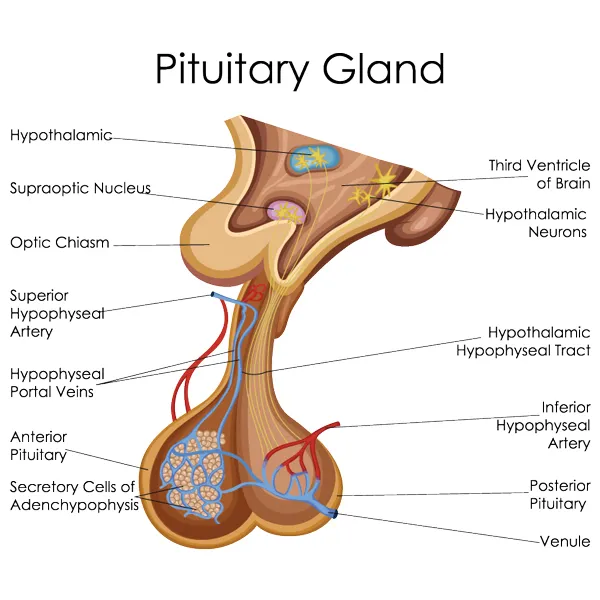
The pituitary gland is located in the middle of the skull base under the brain. It is nested in the “sella turcica” (Turkish saddle) at the top part of the nasal cavity in the sphenoid sinus. Therefore, the pituitary gland is located at the border of the brain and the nasal cavity.
It controls other endocrine glands and is, therefore, called an “orchestra conductor” of the endocrine system.
The pituitary gland has two parts that have different functions. The front part, or adenohypophysis, produces and releases several hormones:
- GH (growth hormone) is the hormone responsible for the growth and development of the bone and several other tissues.
- TSH (thyroid stimulating hormone) is a single hormone controlling the function of the thyroid gland. Its direct action on the gland is to stimulate it to produce more thyroid hormones.
- ACTH (adrenocorticotropic hormone) is a hormone stimulating adrenal glands to make more steroid hormones like cortisol.
- LH (luteinizing hormone) and FSH (follicle stimulating hormone)— in both women and men, these hormones are necessary for the proper function of the reproductive system.
- PRL (prolactin) is a hormone stimulating milk production by breast tissue during the breastfeeding period.
The back part or neurohypophysis stores and releases vasopressin (AKA antidiuretic hormone —controls water balance) and oxytocin (controls uterus contraction during delivery). Oxytocin is also known as a “cuddle hormone” or “love hormone” since it is released when people make social bonds.
The pituitary gland itself is controlled by the part of the brain called the hypothalamus, located just above the gland. The anatomical relationship between the pituitary gland and the hypothalamus is unique. The pituitary stalk is an anatomical connection between the hypothalamus and the pituitary. Hormones of neurohypophysis, like oxytocin and vasopressin, are produced in the hypothalamus and delivered to the pituitary via the stalk. Also, venous blood escaping from the hypothalamus does not enter the systemic circulation. Rather, it flows to the pituitary gland through the pituitary stalk. Therefore, control hormones released by the hypothalamus can directly reach the pituitary. The integrity of the pituitary stalk is essential for normal pituitary function.
What are the types of pituitary adenoma?
Pituitary adenomas are classified either on the basis of their size or hormone status.
Based on the size of the adenoma:
- Microadenoma is a tumor with a size of less than 1 cm
- Macroadenoma is a tumor of more than 1 cm
Based on the hormonal status of adenoma:
- Hormone active adenoma:
- Prolactinoma
- Tireotropinoma
- Corticotropinoma
- Gonadotropinoma
- Somatotropinoma
- Hormone inactive adenoma.
What are the symptoms of pituitary adenoma?
Pituitary adenoma clinically presents with endocrine disturbance and/or compressive effect on near structures.
Endocrine disturbances depend on the hormonal status of the adenoma. If the tumor is producing an extra amount of hormone (hormone active adenoma), usually symptoms are related to an excess of particular hormone:
Prolactinoma – usually presents with galactorrhea — i.e., abnormal milk or milk-like substance discharge from the nipples. In women, the menstrual cycle usually is irregular. In men, libido and erection are diminished.
Thyreotropinoma- excess of TSH stimulates the thyroid gland to produce and secrete more thyroid hormones. The patient develops typical symptoms of hyperthyroidism.
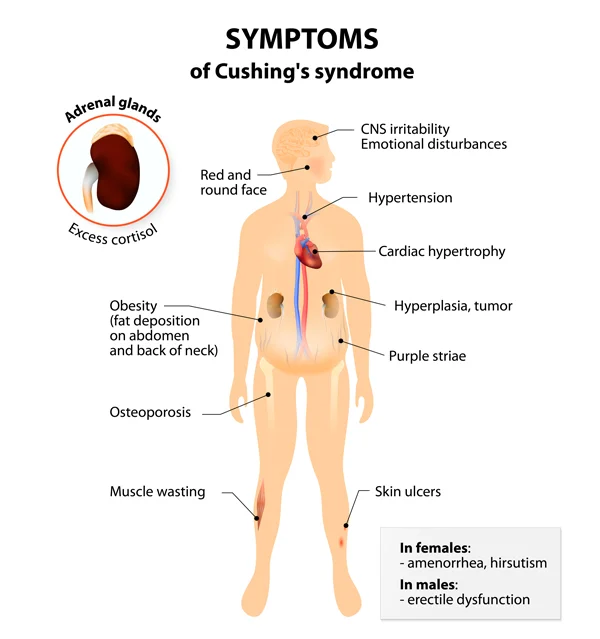
Corticotropinoma – increased ACDH stimulated adrenals to synthesize and release excessive amounts of steroid hormones. This usually leads to Cushing’s disease. On typical presentation, the patients develop obesity, hypertension (high blood pressure), and hyperglycemia (increased sugar in blood).
Gonadotropinoma is a type of pituitary adenoma producing either FSH or LH. Despite increased levels of these hormones, ovaries, and testes are not stimulated. This type of hormonal excess may not be symptomatic at all. If there are symptoms, usually they are related to reproductive function suppression. Infertility, loss of libido, and menstrual disturbances are usual symptoms.
Somatotropinoma presentation is different in children and adults. Since children are capable of growing, an increased amount of growth hormone produces abnormal growth — a condition known as gigantism. In adults, only small bones are growing. Usually, hands, legs, and face are affected, leading to acromegalia.
In addition to hormonal hyper-secretion symptoms, the pituitary adenoma may cause compression of the normal pituitary gland and lead to hypopituitarism — i.e., loss of normal pituitary function.
Another group of symptoms related to pituitary adenoma is caused by its mass effect. In other terms, growing tumors may compress nearby structures and cause neurological deficits. Optic nerves pass just above the pituitary gland and are most commonly affected, which leads to loss of vision. Typically, optic chiasm is compromised, causing loss of vision on the sides. These patients usually complain of narrowing of their visual fields. The presence of loss of vision is very important since it is considered one of the most important indications for surgery. If the tumor extends sideways, it may invade the cavernous sinus. Fine nerves passing inside the cavernous sinus may become compressed and compromised, leading to double vision. In rare cases, tumors may reach a gigantic size, invading the brain. Usually, seizures and/or hydrocephalus can be seen in these cases. Sometimes, the tumor grows downward toward the nasal cavity. It may remain silent for a long time because a nasal cavity is big enough to accommodate a growing tumor. Eventually, a nasal cavity may become obstructed, leading to apnea.
A pituitary tumor is slow-growing, allowing nearby structures to adapt to compression by the tumor. Yet there, in some cases, pituitary apoplexy may develop, leading to rapid tumor expansion. This condition is caused either by bleeding into the adenoma or an ischemic event causing tumor swelling. In any case, expanding tumor mass compresses the optic nerve and normal pituitary, causing loss of vision and hypopituitarism. Pituitary apoplexy is an emergent condition requiring prompt removal of the tumor to relieve the pressure from the optic nerves and preserve vision. Delays in surgical procedures may lead to permanent loss of vision.
How is the pituitary adenoma treated?
There are endocrinological and neurosurgical perspectives involved in the treatment of pituitary adenomas. From the endocrinological perspective, it is important to restore the body’s hormonal balance. Neurosurgeons, on the other hand, focus on relieving the pressure from the neural structures. Therefore, usually, these patients are treated by a team of endocrinologists and neurosurgeons.
Prolactinomas can be initially treated with medical treatment. Dopamine agonist drugs can suppress tumor growth and relieve mass effects. However, there are several handicaps of medical treatment. First, in some instances, this therapy fails to control tumor growth. Second, patients may not tolerate side effects of the medication. Third, dopamine agonist therapy makes tumors fibrotic and difficult to remove surgically. Another handicap of the medical treatment is a significantly increased risk of pituitary apoplexy. All patients receiving dopamine agonist therapy should be instructed about this complication, and they should immediately seek neurosurgical intervention in cases of sudden vision loss.
Somatotropinomas are usually treated with surgery since complete removal leads to a cure. Residual tumors or adenomas not suitable for surgical removal are treated with somatostatin therapy. This synthetic hormone inhibits the secretion of growth hormone from the tumor.
Cortictotropinomas are challenging tumors since they may be too small to be detected by MRI. Additional tests and even explorative surgery may be required to identify the location of these tumors. Another aspect of corticotropinoma surgery is the stormy post-operative period. These patients have increased level of steroid hormones, which drops significantly after surgery. Therefore, these patients may experience significant steroid withdrawal symptoms post-operatively.
Gonadotropinomas and hormonally hormonally inactive tumors are not treated unless there is a mass effect. There is no conservative treatment available for these types of pituitary adenoma, and surgery is the only choice.
Surgery for pituitary adenomas is usually performed from the nasal cavity and is considered one of the most difficult neurosurgical procedures. The surgeon may use either a microscope or endoscope to approach and remove the tumor. In recent years, a growing number of neurosurgeons have used endoscopes for pituitary surgery. The nasal cavity is very narrow and has an irregular shape, making surgical manipulation difficult. Additionally, the pituitary gland is located at the deepest part of the nasal cavity, inside the sphenoid sinus. During surgery, the sphenoid sinus is exposed from the nasal cavity. Afterward, by opening the floor of the sella, the tumor is visualized and removed.
There are several hurdles to pituitary surgery. Carotid arteries pass on each side of the pituitary gland and pose significant problems for the surgeon. Another important aspect is the possibility of cerebrospinal fluid leakage. Normally, the pituitary gland and adenoma are separated from the brain by a thin membrane called diaphragma sellae. This membrane may be damaged during surgery, leading to cerebrospinal fluid leakage from the nose — rhinorrhea. Since the nasal cavity is an infected area, the CSF leakage may cause meningitis, which is a potentially life-threatening condition.