What is the lumbar disc herniation?
Lumbar disc herniation is a condition when degenerated intervertebral disc material slips into the spinal canal, causing compression of the nerve roots.
What is the structure of the lumbar spine?

The human spine is the major supporting structure in the body. It is composed of vertebral bones and joints connecting them. The spine is arbitrarily divided into four parts: cervical, thoracic, lumbar, and sacral. The lumbar spine comprises five lumbar vertebrae and joints between them. These joints provide mobility to the spine. Each vertebral bone is connected to its neighbor via three joints – two facet joints and intervertebral disc.
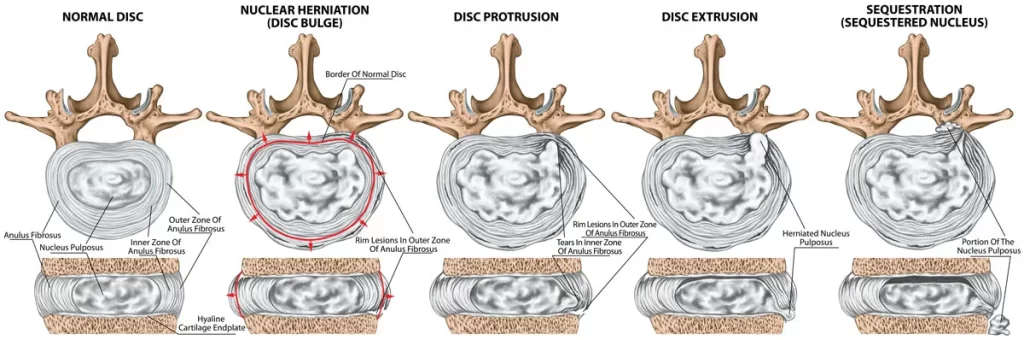
The disc joint is the principal one and provides much of the mobility and load-bearing capacity. It is composed of a core gelatinous component called nucleus pulposus (or simply nucleus) and strong external fibrous ring – annulus fibrosus. The nucleus is very rich in water and is very elastic. It provides cushion for the bones as well as allows bones to move. Disc joint does not have blood vessels. Oxygen and chemicals diffuse passively from and to neighbor vertebral bones. In other words vertebra provide nutritional supply for disc joints. Facet joints are also very important for normal spine function. They restrict motion and prevent vertebra from slippage.
What is disc degeneration and how it leads to lumbar disc herniation?
Disc degeneration is the principal disease leading either to herniation or canal stenosis. Until today we do not fully understand the cellular and molecular mechanisms of disc degeneration. It seems that degeneration is linked to mechanical load. Overweight, tall people are prone to disc degeneration. Occupational heavy lifting leads to accelerated disc degeneration. Smokers have higher chances of developing this disease. Children, teenagers and young adults do not have this disease unless there is major predisposing factor.
Basically evidence shows that degenerative disc disease is a cumulative one. It develops due to dynamic mechanical load on the joint and the inability of the joint to repair itself. Disc degeneration is solely nucleus pulpous disease. As a result elastic, viscous, hydrated nucleus desiccates, shrinks, wears off, and fragments to pieces. Initial stage of degenerative disc disease is called “black disc disease”. Normal nucleus is rich in water and therefore appears bright (white) on T2W MRI images. Dehydration changes disc’s MRI appearance from white to black.
Damaged nucleus loses its mechanical properties and cannot hold the load, and patients start to feel low back pain. Lower back pain is one of the early signs of disc degeneration. In some cases, nucleus breaks down to fragments. One of these fragments can make a tear in the annulus and slip out. This condition is called lumbar disc herniation. Therefore, lumbar disc herniation is not an independent disease, rather it is a consequence of degeneration. Ruptured disc fragment bulges outward and compresses the nerve root passing nearby. This condition is called lumbar radiculopathy. Nerve roots provide innervation to the leg and therefore symptoms of radiculopathy include like pain, numbness, and weakness in the leg.
There are various stages of lumbar disc herniation. At the first, the degenerated nucleus cannot maintain its spring like action and maintain normal disc height. As a result, vertebral bones get closer and annulus fibrosus diffusely bulges out due to mechanical load. Later, a piece of degenerated nucleus may slip between annulus fibers and make local disc protrusion. With further advancement, disc herniation tears the annulus and nests under posterior longitudinal ligament. This stage is known as extrusion. Rarely, slipped fragment may rupture posterior longitudinal ligament, migrate into the spinal canal and completely lose connection with the disc joint. This condition is know as sequestration of the ruptured disc fragment.
What is lumbar stenosis and how it develops?
Degeneration does not always result in lumbar disc herniation. In fact, most of the times damaged nucleus slowly wears off. In other cases fragmented parts remain inside the disc joint without herniation. With time, the joint collapses under body weight. Such gradual loss of physiological disc height leads to spinal stenosis via several mechanisms that should be explicitly explained.
- Bulging. As noted above healthy nucleus acts like a spring and spreads vertebral bodies apart. This action is necessary to maintain normal disc height. With weakening of the nucleus due to degeneration disc height progressively diminishes resulting in outward bulging of the annulus fibrosus and posterior longitudinal ligament. As a result spinal canal narrows.
- Ligamentous hypertrophy. With loss of nucleus pulpous, adjacent vertebra become slightly unstable. Therefore other supporting structures have to enlarge in order to restore the stability. Ligamentum flavum is one of them and its hypertrophy is a compensatory mechanism for disc degeneration. Unfortunately, ligamentum flavum hypertrophy causes significant narrowing of the spinal canal.
- Loss of intervertebral foraminal height. Degeneration causes disc collapse which brings vertebral bones closer. As a result the height and cross sectional area of intervertebral foramina drastically decreases which leads to spinal nerve root impingement.
- Facet hypertrophy. Under physiological conditions facet joints do not take much of the load. However, with loss of disc function they have to compensate and take much of the load. As a result of increased mechanical stress facet joints suffer and get damaged. Also facet bones become larger to hold the weight. Facet hypertrophy further narrows the spinal canal and particularly intervertebral foramina. In this context, hypertrophy of the superior facet is called “superior facet syndrome”. In this condition enlarged superior facet of the lower vertebra causes compression of the exiting nerve root. Another clinical scenario is “lateral recess syndrome”. In this condition hypertrophic facet bone causes narrowing of specific gutter known as lateral recess. This gutter contains traversing nerve root which is compromised in lateral recess syndrome
- Osteophyte formation. Normally, mechanical load from body weight is evenly distributed through the disc space due to visco-elastic nature of the healthy nucleus. Degeneration cause uneven load distribution and triggers excessive bone growth. Such extra bone protrusions may narrow either the spinal canal or neural foramina contributing to lumbar stenosis.
- Degenerative spondylolisthesis and retrolisthesis. In some cases, disc degeneration causes loss of vertebral alignment. If supporting ligaments and facet joints cannot compensate for loss of stiffness vertebral bones may lost its normal alignment. Degenerative instability in the affected disc may cause vertebral bone to slip forward (spondylolisthesis or anterolisthesis) or backward (retrolisthesis). Such misalignments contribute to stenosis and may compress or stretch nerve roots.
- Kyphosis, hyperlordosis and scoliosis. Normally, lumbar spine has a curve forward which is known as lordosis. The spine generally has alternating forward and backward curves which gives characterizing double S shaped appearance when looking from side. However the spine is pretty straight from front (or back). Severe disc degeneration, particularly at multiple levels may affect the shape of the spine. It may manifest as loss of lordosis – “flat back syndrome” or lumbar kyphosis, exaggerated lordosis – hyperlordosis, and sometimes loss of coronal balance leading to scoliosis.
What are the symptoms of lumbar disc herniation?

Symptoms of the disease depend on the duration and extent of the process. Degeneration and black disc disease alone causes low back pain. The mechanical nature of the pain is very specific. Pain is aggravated by increased load and relieved by resting. Bending forward combined with heavy lifting may trigger an acute low back pain attack. Usually, these attacks last from several days to several weeks and respond very well to resting and pain medication. Pain might also be aggravated by cold, and that is why it is usually worse during winter season.
The presence of leg pain indicates nerve root compromise and is an early sign of radiculopathy. Usually, this type of pain starts in the lower back region and radiates to the leg. The presence of pain in one extremity is a common, yet both legs may be affected, too. The extent of leg pain depends on the degree of nerve root impingement. Each nerve has a specific unique innervation area and physicians may diagnose the affected nerve root by asking the patient to localize leg pain. Advanced compression causes nerve function compromise and results in loss of sensation (hypoesthesia) and weakness of the leg muscles (paresis). These symptoms are known as neurological deficits and should alarm patients and physicians. Delays in diagnosis and treatment of neurological deficits usually cause permanent loss of neurological function.
Lumbar stenosis causes a specific set of symptoms different from lumbar disc herniation. Since the process is very slow, classical radiculopathy is not usually present. Patients often experience “neurogenic claudication,” – which is characterized by the inability to walk long distances without rest. As the disease progresses, walking distances become shorter, significantly compromising the patient’s quality of life. Usually, both legs are involved, though asymmetrical involvement is frequent.
How is the diagnosis of lumbar disc herniation made?
The diagnosis of lumbar disc herniation is done by meticulous clinical examination and radiological assessment. In typical clinical scenario clinical examination raises suspect and radiological verification confirms clinical diagnosis and provides information about the extent and stage of the disease.
Clinical Examination
History of the disease and physical examination are undoubtedly the most crucial parts of the patient’s evaluation. Not only is clinical examination important for the evaluation of neurological status, but it also provides crucial information for a correct treatment plan.
History of the disease
History provides valuable clues from very beginning of communication. One of the most consistent features of degenerative lumbar disease is mechanical low bak pain. The pain is either provoked or worsened by mechanical stress like standing, walking, sitting, heavy lifting or bending forward or backward. Non-mechanical low back pain should raise suspicion of other diseases. Another typical feature of pain is cold intolerance. Patients however may not mention it during conversation unless specifically asked.
The presence of leg pain is the sign of nerve root involvement. However, it does not necessarily mean nerve root impingement. Slight compression irritates nerve and does not usually affect its physiology. However, if patient mentions numbness and weakness the physician must be alerted about the possibility of serious nerve root compression.
In many cases patients already know their diagnosis before visiting doctors. This is a typical situation when patients are referred or have long history of disease with multiple treatment attempts. Some of them may have prior surgeries.
Clinical Examination
Clinical examination of patients with known or suspected degenerative lumbar spine disease should include neurological examination and several specific tests. Neurological examination is basically focused on looking for sensory and motor deficits. As mentioned above, every spinal nerve root provides innervation to specific skin area and muscles in the leg. Therefore careful neurological examination may reveal which nerve root or roots might be compromised. Of course the presence and degree of neurological deficit are key factors in formulating the treatment plan. Patients with minimal or no neurological deficits may undergo conservative treatment while significant or rapidly evolving neurological deficits require prompt surgical intervention.
One of the most commonly used test for lumbar disc herniation is straight leg raise (SLR) or Laseque’s test. During this test patient lays supine and the examiner passively elevates the leg. If pain is induced by this maneuver the test is considered positive. The main mechanism behind this test is tension on the sciatic nerve and lower lumbar nerve roots. There several modifications of this test including contralateral SLR when pain occurs in the affected leg with unaffected leg elevation. Another variation include femoral nerve tensile test during which femoral nerve and upper lumbar nerve roots are stretched.
Another important part of clinical evaluation is local examination of the lower back area. Manual palpation or gentle tapping of the affected area may reveal exact source of the pain. Quite frequently clinician encounter paravertebral muscle spasms. These involuntary contractions are believed to originate as a response to low back pain and instability and quite typical for degenerative lumbar spine disease.
Clinical examination of lumbar spinal stenosis patients usually do not reveal much. This is quite striking to degree of their complaints. Neurological examination is normal or near normal, SLR or other tensile test negative and there is minimal or absent tenderness in the low back area. Such disparity between abundant complaints and fair clinical findings is very typical in spinal stenosis.
Radiological evaluation
Radiological evaluation is a very important part of assessment. Modern radiological tools can precisely diagnose degenerative lumbar disease. They are indispensable for mapping out treatment plan. There are several radiological modalities used for degenerative spine disease diagnosis. Each modality has its own advantages.
MRI
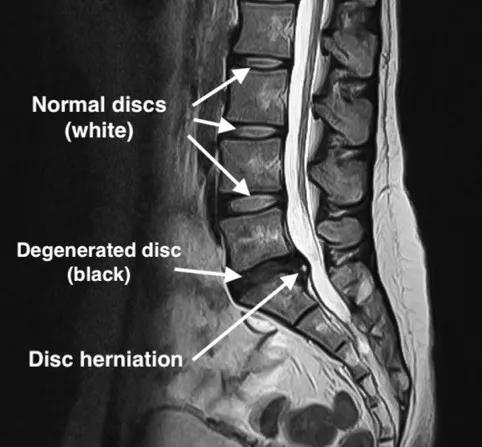
MRI of the lumbar spine is the diagnostic test of choice. It provides close-up highest resolution images of spine in all three planes. Multiple MRI sequences help to visualize pathology on from various perspectives.
One of the striking advantages of MRI is ability to visualize the disc joint and ongoing degeneration. In fact the term “black disc disease” originates from MRI appearance of the degenerated disc. MRI clearly shows disc degeneration, herniation, spinal stenosis. Also it may demonstrate other pathologies like fracture, inflammation, tumor etc.
X-ray
X-rays provide good information about bones specifically, lumbar spine alignment, presence of deformity, bone spurs, narrowing of the disc spaces, vertebral slippage, etc. It cannot visualize soft tissue like disc joint itself or disc herniation per se. One of the advantages of X-ray that it can be taken while standing and in various conditions like flexing or extending. Such dynamic evaluation might be useful in some selected cases.
CT scan
CT also utilizes X-rays but with much higher resolution. Like X-ray it is suitable for bone visualization. Fractures, misalignments, bone erosions and osteophytes are much better demonstrated by CT scan. It also possible to reconstruct 3D images from raw scan for better visualization.
EMG and nerve conduction studies
EMG, nerve conduction, and evoked potential studies can be performed in some cases to confirm the presence of radiculopathy if the diagnosis is doubtful. However, their practical usefulness is limited. These studies are especially helpful in distinguishing radiculopathy from peripheral nerve compression syndromes.