Key Facts on DISH Disease
- DISH, which stands for Diffuse Idiopathic Skeletal Hyperostosis (aka Forestier disease), is a systemic disease affecting skeletal system and characterized by formation of extra bones (osteophytes) at the enthesis sites. Enthesis in medical literature refers to anatomical region where connective tissue (ligament, tendon, joint capsule etc) attach to the bone. Therefore DISH is enthesopathy.
- DISH primarily affects the spine and manifests by formation of osteophytes along the anterior longitudinal ligament. Although the spine is mostly affected, extra spinal manifestations in pelvis and extremities are not uncommon. Interestingly, sacro-iliac joints are not affected in DISH.
- The exact cause of DISH is unknown, but combination of genetic, metabolic, inflammatory and behavioral factors are likely to cause the disease. DISH shares similarities with other skeletal conditions like ankylosing spondylitis and osteoarthritis but differs in several aspects.
- DISH is a disease of elderly, affecting patients in their 60s and 70s. Males are affected more than females. It is estimated that about 10% of elderly men may have DISH. However, in severe familial cases some patients may develop this condition in their 30s.
- The condition primarily affects the thoracic and cervical regions of the spine, leading to pain and stiffness in these areas. Osteophytes along the anterior aspect of the spine may compress vital structures like esophagus or sympathetic nerves.
- DISH is diagnosed primarily through imaging studies, with X-rays revealing the formation of bony outgrowths or osteophytes along the spine and in other regions.
- DISH can lead to significant mobility issues and potentially qualify as a disability in severe cases.
In this article, we will explain what diffuse idiopathic skeletal hyperostosis (DISH) is and delve into how new bone formation contributes to clinical symptoms. We’ll also explore the differences between DISH and idiopathic arthritis of other types, as well as spondylitis and DISH, and how this condition can impact daily life.
What is DISH Disease?
DISH, also known as diffuse idiopathic skeletal hyperostosis, is a common bone disease that manifests by formation of calcifications and extra bone tissue at insertion points of ligaments and tendons which is known as enthesis. DISH leads to stiffness and discomfort, often resulting in back and neck problems. This spine condition can lead to significant stiffness and pain, resembling arthritis in its symptoms, which has led some to use the term DISH arthritis.
Despite its clinical manifestations, the exact cause of DISH remains unclear, hence the designation “idiopathic” in its name, indicating an unknown origin. Unlike other forms of bone diseases, DISH specifically targets the areas where ligaments and tendons attach to the spine (enthesis), leading to bone growths that can restrict movement.
Is DISH disease a disability?
The question of whether DISH qualifies as a disability depends on the severity of the symptoms and the extent of impact on an individual’s daily life. For some patients with DISH, the condition might lead to significant mobility issues, severely affecting their ability to perform daily tasks, thus potentially qualifying as a disability.
Forestiers Disease: Another Medical Term for DISH
Forestier’s Disease is an alternative name for DISH, named after the French physician Jacques Forestier, who first described the condition in 1950 under the name “senile ankylosing vertebral hyperostosis”. 1 While “Forestier’s Disease” is sometimes used interchangeably with DISH, it is important to note that this term specifically highlights the historical contribution of Dr. Forestier to the understanding of this bone disease. In some medical circles, the condition might also be referred to as “Forestier’s Syndrome” or, less commonly, “Forestier-Rotes-Querol Syndrome,” acknowledging the collaborative efforts of Forestier and his student Jaume Rotes-Querol in identifying this unique medical condition.
Ankylosing Hyperostosis
Ankylosing hyperostosis of the spine is another term that has been used historically to describe DISH or Forestier’s disease. It emphasizes the excessive bone growth along the anterior aspect of the spine, particularly in the thoracic region. This term is less commonly used today, and the preferred terminology is DISH or diffuse idiopathic skeletal hyperostosis.
How serious is DISH disease?
The severity of DISH disease can vary significantly among individuals. In some cases, it may present as mild discomfort in the back or neck, with little impact on daily activities. However, as the disease progresses, it can lead to more serious complications, such as significant loss of mobility in the spine, pain, and difficulty swallowing. These complications can severely affect the quality of life for patients with DISH, making it challenging for them to perform routine tasks. The seriousness of DISH disease is influenced by factors such as the extent of bone growth, the areas of the spine affected, and the presence of other health conditions.
Spinal Segments Affected by DISH
DISH primarily affects the thoracic and cervical regions of the spine, with involvement of the lumbar region being less common. Sacro-iliac joints are spared in DISH, which is the major feature distinguishing it from ankylosing spondylitis.
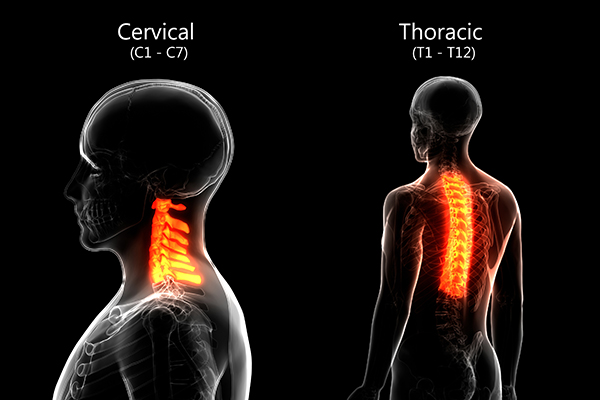
DISH in the Thoracic Spine
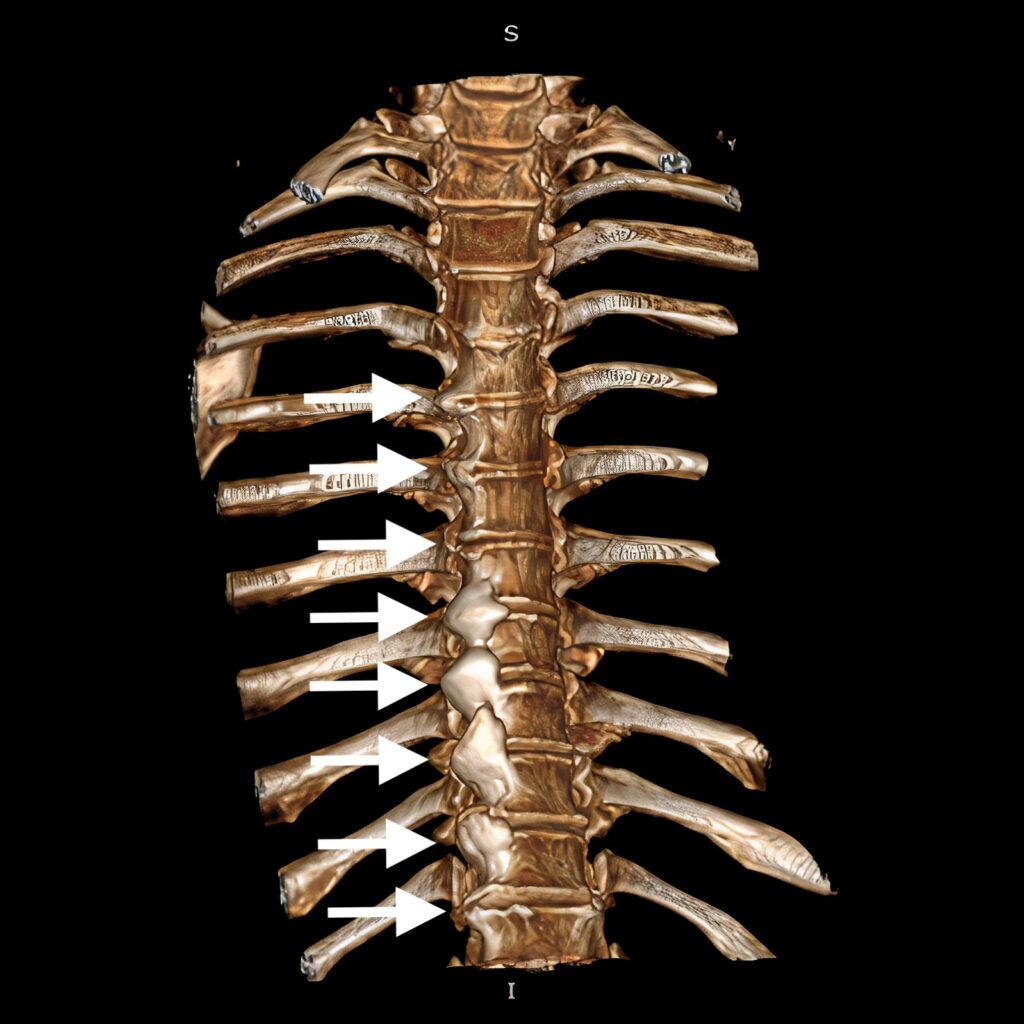
DISH in the thoracic spine, or thoracic DISH, is a most common manifestation of the disorder. This skeletal condition leads to the formation of bone spurs (osteophytes) on the anterior (front) surface of the spine along anterior longitudinal ligament. The thoracic spine is particularly susceptible to DISH because of its limited mobility compared to other parts of the spine. Usually DISH is more severe in the lower part of thoracic spine (T5-11). Characteristic feature of lower thoracic osteophytes is their asymmetric appearance i.e., they develop exclusively on the right side. It is not known why the right side is affected more but some researchers suggested that the presence of aorta on the left side inhibits new bone formation. 2 This hypothesis has been confirmed in a recent study. 3

Aorta changes its position anterior to spine in the lumbar region and therefore osteophytes in this region develop bilaterally (i.e. on both left and right sides). It is believed that pulsations from aorta interfere with deposition of calcium and subsequent ossification. Upper part of thoracic spine – T1-5 levels, is affected less than the lower part. However, if DISH is present in the upper part bone spurs tend to grow symmetrically due to absence of aorta.

Bone spurs grow out of vertebral end-plates. Intervertebral disc joints are not affected. Osteophytes from upper and lower vertebra may coalesce and form bone bridges along right anterior surface. As a result, vertebral bones fuse which significantly reduces spine mobility. Typically, several vertebral bones merge into one long immobile segment. Radiologically this segment has classic wave-like appearance on X-ray or CT scan.

Individuals with thoracic spine DISH experience symptoms such as back pain, reduced range of motion, and in severe cases, difficulty breathing due to the involvement of the rib cage. The pain is felt in the midline along the spine or on side of the spine. Bone spurs may compress the nearby structures and cause their dysfunction. Although rare, compression of esophagus has been reported. 4 Much more commonly osteophytes compress sympathetic splanchnic and cardiopulmonary nerves passing along the anterior surface of the thoracic spine. 2 Compression of sympathetic nerves may produce significant autonomic type pain. The pain is intensive, frequently associated with burning. Other sympathetic phenomena like warming, coldness, and sweating are also common. Sympathetic nerves are innervating internal organs and their compression may may produce number of symptoms related to internal organs’ dysfunction such as gastrointestinal upset, abdominal pain, cardiac arrhythmia. 5
Loss of spine’s flexibility and increased stiffness is probably the most significant feature of DISH. The range of physiological motion per motion segment is lower than in cervical and lumbar regions. However, higher number of thoracic vertebra (12 vs 7 in cervical and 5 in lumbar) make compound effect i.e., small individual motions add up and make substantial overall range of motion. 6 Additionally, DISH may extend to cervical and lumbar segments and cause very significant overall motion restriction. Loss of spine’s mobility is a significant factor contributing to morbidity of disease. The patients however may not relate stiffness to disease and consider it as a part of aging. Increased rigidity of spine has two crucial consequences
- Increased dynamic load to other motion segments and subsequent accelerated degeneration. It is well-known that decreased motion in one segment leads to compensatory increase in neighbor joints. As result the dynamic load to these levels increase and intervertebral disc joints degenerate faster. 7 Disc herniations, stenosis and segmental instability due to higher stress is frequent finding in DISH patients, especially at the lower part of the fused segment. 8 As a result of accelerated degeneration compression of spinal cord and nerves are not uncommon in DISH patients.
- Increased risk of spinal fractures even with minor trauma. Fused vertebral bodies make a long cantilever arm. Like a longer stick which can be broken much easier than a short one this long rigid segment is prone to fracture even with low energy impacts. 9
DISH in the Cervical Spine
DISH of the cervical spine is another common manifestation of the disorder. This form of the disease leads to the calcification and ossification of anterior longitudinal ligament. Newly formed osteophytes bulge out the vertebral bones and frequently merge to form bone bridges. In some cases these bridges span over several vertebra and fuse them. Unlike lower thoracic osteophytes these bone spurs are fairly symmetric. The cervical spine is crucial for supporting the head and maintaining its movements, so DISH in this segment significantly impacts individual’s ability to perform daily activities.
Symptoms of cervical DISH include neck pain and reduced neck mobility. In severe cases osteophytes may grow up so extensively that they compress esophagus and/or trachea which lie directly in front of the spine. In these situations patients experience difficulty swallowing (dysphagia) or breathing due to external mechanical obstruction. 10
Fused cervical vertebra form one long immobile segment. As a result the upper and especially the lower intervertebral disc joints experience higher dynamic load. This extra mechanical stress accelerates degeneration which already present in many elderly people. The degree of degeneration may be so severe that spinal cord (myelopathy) and or cervical spinal nerve roots (radiculopathy) may get compressed. Symptoms of degenerative myelo- and radiculopathy include pain, numbness, weakness, in the arms and legs as well as unsteady gait and urinary incontinence in severe cases.
DISH in the Lumbar Spine
Although not as frequent as in thoracic and cervical segments diffuse idiopathic skeletal hyperostosis may affect the lumbar spine as well. Like in thoracic and cervical spine calcification and ossification of anterior longitudinal ligament is hallmark of the disease. Due to more central position of the aorta, the osteophytes tends to be more symmetric in the lumbar spine. Extra bone protrusions may fuse adjacent lumbar vertebra and lead to decreased immobility. Considering that the lumbar spine is quite flexible and is the major load bearing structure of the body such restriction puts extra mechanical stress to unaffected levels speeding up their degeneration. 11

In many cases lumbar DISH co-exists with lumbar degenerative stenosis. Spine surgeons may not recognize or ignore DISH before surgery. However, the presence of DISH have been linked to poorer surgical outcomes in patients undergoing surgery for with lumbar stenosis. 12 Therefore recognizing DISH preoperatively is very important for spinal surgeons.
Extraspinal DISH
It should be kept in mind that DISH is systemic disease. Although spine is most commonly affected skeletal structure other bones may be involved as well. Pelvis and extremities are frequently affected but usually do not produce many symptoms
- Pelvis. Calcifications and ossifications of the pelvic and sacral ligaments are typical. Iliolumbar, sacro-tuberous and sacro-iliac ligaments show signs of calcification. Other pelvic manifestations include development of osteophytes, irregular projections and bridging osteophytes over pubic symphysis. 13
- Extremities. Upper and lower extremity entheses are frequently affected. Common sites include olecranon, patella, metacarpal bones as well as phalanxes. It should be noted that DISH is frequently seen in association with osteoarthritis (OA) which is also characterized by bone osteophytes in hands. However, the size and number of these extra bone protrusions is higher in patients with DISH and OA than with OA alone.
Diffuse Idiopathic Skeletal Hyperostosis Causes
The exact causes of diffuse idiopathic skeletal hyperostosis (DISH) remain unknown, which is reflected in the term “idiopathic” in its name. However, researchers have identified several factors that may contribute to the development of the condition.
- Genetic factors. The research regarding genetic factors involved in DISH has revealed several candidate molecules and pathways. COL6A1, FGF2, RSPO4, LEMD3, PPP2R2D, BMP4, ALK2, ENT1 are all candidate genes implicated in pathogenesis of DISH. 14
- Age and gender. DISH is predominantly elderly disease and more common in males. Increased incidence of DISH with aging is well reported. People over 70 are particularly prone to DISH but in familial cases patients may get affected even in their 30s.
DISH Disease Symptoms
Generally, the symptoms of DISH vary depending on the location and severity of the condition. Spine involvement is universal and increased stiffness is hallmark of the disease. However, since DISH is a chronic disease and takes many years to develop, patients may be unaware of their condition and/or relate it to aging. As DISH progresses, this stiffness can result in substantial loss of range of motion, making daily activities difficult.
Pain in the affected area is a very frequent symptom. In fact, the pain is the most important factor affecting the quality of life and forcing patients to seek medical treatment. Usually, the pain is located directly in the midline over the spine or paramedian (i.e. the area immediately left or right to the midline). Initially pain may be alleviated by non-steroidal anti inflammatory drugs (NSAIDs) but later becomes resistant to them. If DISH affects pelvis and/or extremities affected entheses may become painful as well.
The overgrowth of osteophytes can lead to compression of nearby structures and produce symptoms. In cervical spine compression of esophagus is typical and leads to dysphagia. In thoracic and lumbar spine osteophytes may compress sympathetic nerves and result in chronic excruciating sympathetic pain and/or internal organs dysfunction.
DISH Diagnosis and Tests
A comprehensive DISH diagnosis typically involves a combination of medical history review, physical examination, and radiographic analysis. The diagnosis of DISH is primarily confirmed on imaging studies. The hallmark sign of DISH on imaging is the presence of calcification along the anterior and lateral border of spine, particularly noticeable in the thoracic region. The diagnosis is confirmed when specific criteria are met, such as the continuous calcification along four or more consecutive vertebrae and by the absence of sacroiliac joint involvement– so called Resnick and Niwayama criteria. 15 These criteria are very efficient in establishing the disease and differentiating it from other, similar conditions. Recently however, a modified version of these criteria have been proposed by Oudkerk et al. 16 These criteria are important for healthcare professionals to differentiate DISH from similar diseases that can mimic DISH radiographic findings.
DISH X-ray
An X-ray is a crucial tool in the diagnosis of diffuse idiopathic skeletal hyperostosis. Before advent of computerized tomography (CT) it was the only method to establish the diagnosis. In fact, X-ray has good diagnostic sensitivity and specificity to DISH. It typically reveals characteristic changes in the spine, such as the formation of bony outgrowths and calcifications along the anterior longitudinal ligament. These changes are most commonly seen in the thoracic spine but can also occur in the cervical and lumbar regions. The X-ray findings of flowing ossification along the spinal ligaments are distinctive for DISH and help differentiate it from other spinal conditions.

Computerized tomography (CT) scan
Although X-ray is an excellent tool for DISH diagnosis it has several limitations. For example visualization of several spiral regions (upper thoracic, thoracic-lumbar junction) may be problematic. Another handicap is its 2 dimensional nature i.e. 3 dimensional object is represented on single surface. CT scan allows much more precise visualization. The 3 dimensional body is scanned slice by slice which can be combined together to reconstruct the image in all 3 planes and even in 3d format. This way the exact shape, size and location of osteophytes can be visualized much more accurately. In fact, new modified criteria proposed by Oudkerk et al based on CT scan. 17
DISH and Related Conditions
Diffuse Idiopathic Skeletal Hyperostosis shares similarities with several other skeletal conditions, making differential diagnosis crucial. Understanding the distinctions between DISH and related conditions is essential for accurate diagnosis and appropriate treatment.
DISH vs. Ankylosing Spondylitis
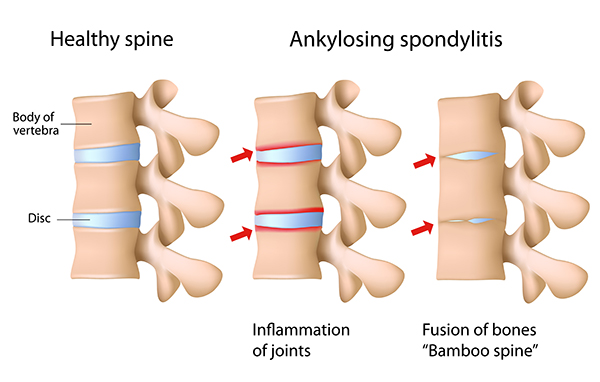
Both DISH and ankylosing spondylitis are conditions resulting in spontaneous spinal fusion, but have distinct characteristics. DISH is characterized by absence of inflammation, calcification along the anterior longitudinal ligament, and absence of sacroiliac joint (SI) involvement (though ligaments around SI joint are frequently calcified). Ankylosing spondylitis (AS), on the other hand, is an inflammatory condition that primarily affects the sacroiliac joints and progresses to spine leading to fusion of the vertebrae. Characteristic feature of AS is symmetric involvement of disc joints leading to typical bamboo spine appearance. Marked spinal deformation is another hallmark of ankylosing spondylitis and is usually absent in patients with DISH.
Disc degeneration
Intervertebral disc degeneration is common condition affecting the spine particularly in elderly. It may have several features resembling DISH. Formation of osteophytes is common in later stages of disc degeneration making it similar to DISH. However, there are several key differences. The most discernible distinction is marked degeneration of the disc joint and narrowing of the disc space in degenerative disc disease. This disc space height on the other hand is well preserved in DISH. Osteophytes in disc degeneration tend to occur in cervical and lumbar regions more where the disease is most pronounced while DISH usually affects thoracic spine. Also degeneration related osteophytes are usually isolated and confirmed to involved discs while DISH associated osteophytes are clustered together. Facet joints are usually spared in DISH while intervertebral disc joint degeneration puts additional load on them and causes hypertrophy.
Although the distinction between DISH and degenerative spine disease is usually clear these two conditions may (and usually) coexist in the same patient. DISH leads to spontaneous fusion of a segment of the spine and accelerates neighbor disc joints’ degeneration. 7 Degenerated disc itself may develop osteophytes which contribute to spinal stenosis. Recognizing DISH as trigger factor for lumbar degeneration is very important since surgical outcomes differ in patients with and without DISH. 12
DISH Prognosis
The prognosis for patients with DISH disease is generally favorable, especially when the condition is diagnosed early and managed effectively. However, the presence of complications such as difficulty swallowing or sympathetic nerve compression can impact the overall prognosis. Regular monitoring and a proactive approach to symptom management are key to maintaining a good quality of life.
How fast does DISH disease progress?
The progression of DISH disease can vary widely among individuals. For many, the disease progresses slowly, and symptoms may remain stable for years. In some cases, the condition may not progress significantly beyond the initial presentation. However, in others, the disease may gradually worsen over time, leading to reduced mobility. Factors such as age, overall health, and lifestyle can influence the rate of progression. Regular check-ups with a healthcare provider are important to monitor the progression of the disease and adjust treatment as needed.
Conclusion: Emerging DISH Treatment Methods- What’s Next?
As our understanding of DISH disease continues to evolve, so too do the treatment methods available to those affected by this condition. While traditional approaches have focused on managing symptoms and maintaining mobility, emerging treatments and surgery methods offer more targeted and effective interventions.
Next Chapter: DISH Disease Treatment — Achieving Permanent Pain Relief Through Surgery
References
- Forestier J, Rotes-Querol J. Senile ankylosing hyperostosis of the spine. Ann Rheum Dis. 1950;9(4): 321-330. https://doi.org/10.1136/ard.9.4.321[↩]
- Nathan H. Osteophytes of the spine compressing the sympathetic trunk and splanchnic nerves in the thorax. Spine (Phila Pa 1976). 1987;12(6): 527-532. https://doi.org/10.1097/00007632-198707000-00003[↩][↩]
- Chen H, Zhou Q, Wang S, et al. Not All Osteophytes Are Located on the Right Side of the Vertebrae in Diffuse Idiopathic Skeletal Hyperostosis: A Quantitative Analysis in Relation to the Position of Aorta. Orthop Surg.2023;15(11): 2881-2888. https://doi.org/10.1111/os.13869[↩]
- Pongmanee S, Rojdumrongrattana B, Kritworakarn N, Sarasombath P, Liawrungrueang W. An unusual presentation of thoracic diffuse idiopathic skeletal hyperostosis (DISH) and video-assisted thoracoscopic surgery (VATS). Int J Surg Case Rep. 2022;93: 106993. https://doi.org/10.1016/j.ijscr.2022.106993[↩]
- Mader R, Dubenski N, Lavi I. Morbidity and mortality of hospitalized patients with diffuse idiopathic skeletal hyperostosis. Rheumatol Int. 2005;26(2): 132-136. https://doi.org/10.1007/s00296-004-0529-y)) etc. Surgical removal of these osteophytes relieve the pressure from splanchnic nerves and provide significant improvement. ((Jankowski J, Pawelczyk A, Radek M. Thoracic osteophyte as a cause of symptomatic greater splanchnic nerve compression. Case report. Neurochirurgie. 2022;68(2): 232-234. https://doi.org/10.1016/j.neuchi.2021.02.017[↩]
- Borkowski SL, Tamrazian E, Bowen RE, Scaduto AA, Ebramzadeh E, Sangiorgio SN. Challenging the Conventional Standard for Thoracic Spine Range of Motion: A Systematic Review. JBJS Rev. 2016;4(4): e51-e511. https://doi.org/10.2106/JBJS.RVW.O.00048[↩]
- Nakasuka M, Morino T, Hino M, Misaki H, Murakami Y, Miura H. Diffuse idiopathic skeletal hyperostosis: A potential factor in the induction of thoracic spondylotic myelopathy. J Orthop Sci. 2021;26(1): 75-78. https://doi.org/10.1016/j.jos.2020.01.009[↩][↩]
- Yamada K, Satoh S, Hashizume H, et al. Diffuse idiopathic skeletal hyperostosis is associated with lumbar spinal stenosis requiring surgery. J Bone Miner Metab. 2019;37(1): 118-124. https://doi.org/10.1007/s00774-017-0901-0[↩]
- Murakami Y, Mashima N, Morino T, et al. Association Between Vertebral Fracture and Diffuse Idiopathic Skeletal Hyperostosis. Spine (Phila Pa 1976). 2019;44(18): E1068-E1074. https://doi.org/10.1097/BRS.0000000000003151[↩]
- Harlianto NI, Kuperus JS, Mohamed Hoesein FAA, et al. Diffuse idiopathic skeletal hyperostosis of the cervical spine causing dysphagia and airway obstruction: an updated systematic review. Spine J. 2022;22(9): 1490-1503. https://doi.org/10.1016/j.spinee.2022.03.002[↩]
- Yamada K, Satoh S, Abe Y, Yanagibashi Y, Hyakumachi T, Masuda T. Diffuse Idiopathic Skeletal Hyperostosis Extended to the Lumbar Segment Is a Risk Factor of Reoperation in Patients Treated Surgically for Lumbar Stenosis. Spine (Phila Pa 1976). 2018;43(20): 1446-1453. https://doi.org/10.1097/BRS.0000000000002618[↩]
- Otsuki B, Fujibayashi S, Tanida S, Shimizu T, Lyman S, Matsuda S. Outcomes of lumbar decompression surgery in patients with diffuse idiopathic skeletal hyperostosis (DISH). J Orthop Sci. 2019;24(6): 957-962. https://doi.org/10.1016/j.jos.2019.09.003[↩][↩]
- Resnick D, Shaul SR, Robins JM. Diffuse idiopathic skeletal hyperostosis (DISH): Forestier’s disease with extraspinal manifestations. Radiology. 1975;115(3): 513-524. https://doi.org/10.1148/15.3.513[↩]
- Dabrowski M, Kubaszewski L. Diffuse Idiopathic Skeletal Hyperostosis of Cervical Spine with Dysphagia-Molecular and Clinical Aspects. Int J Mol Sci. 2021;22(8). https://doi.org/10.3390/ijms22084255.))
- Epigenetic factors. In order to properly function genes should be regulated. Over-expression and under-expression of genes may result in abnormal function. Several epigenetic factors have been hypothesized. DNA methylation, and expression of non coding RNA (ncRNA) specifically micro RNA (miRNA) have been proposed.
- Metabolic factors. The association between obesity, diabetes, hypertension, dyslipidaemia and DISH is well known. However, it is not known whether DISH develops as a consequence of these conditions or due to shared risk factors. ((Mader R, Verlaan JJ, Buskila D. Diffuse idiopathic skeletal hyperostosis: clinical features and pathogenic mechanisms. Nat Rev Rheumatol. 2013;9(12): 741-750. https://doi.org/10.1038/nrrheum.2013.165[↩]
- Resnick D, Niwayama G. Radiographic and pathologic features of spinal involvement in diffuse idiopathic skeletal hyperostosis (DISH). Radiology. 1976;119(3): 559-568. https://doi.org/10.1148/119.3.559[↩]
- Oudkerk SF, de Jong PA, Attrach M, et al, Diagnosis of diffuse idiopathic skeletal hyperostosis with chest computed tomography: inter-observer agreement, Eur Radiol. 2017;27(1): 188-194, https://doi.org/10.1007/s00330-016-4355-x[↩]
- Oudkerk SF, de Jong PA, Attrach M, et al. Diagnosis of diffuse idiopathic skeletal hyperostosis with chest computed tomography: inter-observer agreement. Eur Radiol. 2017;27(1): 188-194. https://doi.org/10.1007/s00330-016-4355-x[↩]