What is the vertebral compression fracture?
Vertebral compression fracture (VCF) is a specific type of spinal fracture when the spinal bone is smashed and deformed due to injury forces.
How does the vertebral compression fracture develop?

Vertebral bone is composed of two types of bone tissue – compact and spongious. Compact bone comprises the outer shell of the vertebral bone. This bone is very robust and provides a shell for the inner portion, which is composed of spongious bone tissue. Spongous bone has a lot of space inside and looks like a sponge. These tiny spaces are filled with bone marrow and venous blood. Unlike other bones, vertebral bones are mostly composed of spongous bone. Therefore, they may suffer from a compression fracture. This fracture is unique because there are no broken parts. Rather, the vertebra is deformed and smashed. Typically, the front part of the bone is cracked and collapsed while the back portion is spared. This condition creates an abnormal angle in the spinal column, causing deformity, i.e., loss of normal shape. If the angle is too much and the fracture fails to heal, the load may lead to progressive collapse, increasing the deformity.
Usually, the vertebral bone is quite sturdy and cannot be fractured easily. Significant force is required to cause a vertebral compression fracture in healthy bone. However, there are several conditions that may weaken the bone. Osteoporosis is a condition frequently affecting older people, especially in women. This is a condition characterized by progressive loss of bone tissue. As a result, bones become weak and fragile. These patients may develop different fractures in their bodies, including vertebral compression fractures. Another common cause of VCF is cancer. Tumors growing inside of the vertebra usually erode it and cause weakening. Therefore, patients with osteoporosis or tumors may develop compression fractures with relatively minor trauma or no trauma at all.
What are the symptoms of vertebral compression fracture?

The main symptom of the vertebral compression fracture is pain. Typically, patients develop the pain right after the moment of fracture. This pain is usually mechanical, i.e., it is worse with a physical load like standing or working. The pain may become chronic and persist several months after the fracture. In some instances, the initial pain is not very intensive, but with progressive collapse, it may become excruciating. Some patients may become wheelchair-bound or even bedridden.
Another symptom of vertebral compression fracture is kyphosis. Since the front part is collapsed more, the spine makes an angle at the site of fracture. This angle causes front bending of the spine, i.e., kyphosis. Kyphosis initially may not be visible; however, with progressive collapse, the deformity may significantly worsen.
Unlike other fracture types, compression fracture usually does not lead to spinal canal compromise and spinal cord compression. Therefore, the patients are usually neurologically intact.
How is the vertebral compression fracture diagnosed?
Physical examination and imaging studies are the two main methods to diagnose vertebral compression fractures. The examination may reveal the exact site of the pain and the presence of deformity. Spine imaging like MRI, CT, or X-rays is invaluable for the diagnosis. These scans can nicely demonstrate the affected bone, degree of collapse, deformity, bone edema, spinal canal status, and many other details.
Usually, physical exam and imaging studies are sufficient, yet if the tumor is present, then additional investigations may be performed to find out the nature of the tumor.
What is the treatment of vertebral compression fracture?
The treatment depends on the duration of symptoms, degree of compression, and presence of additional injuries. In the vast majority of cases, initially, the patients are treated with pain medications and rest. In some cases, physicians may add external casts or orthosis to restrict the spine’s motions temporarily.
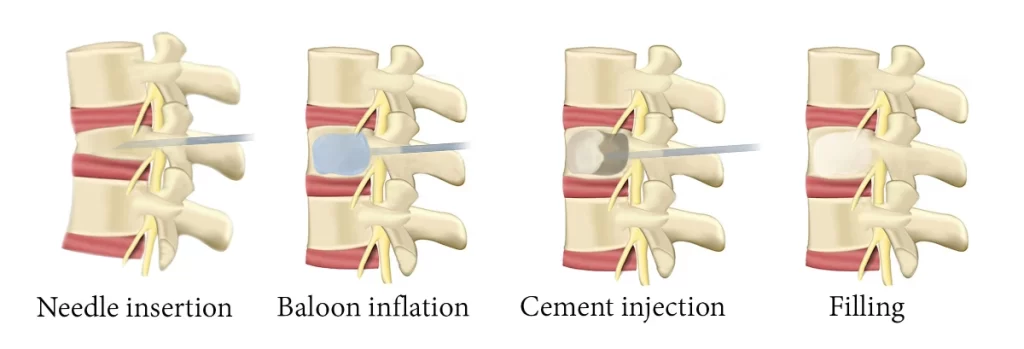
If the pain persists for more than several weeks, surgical treatment should be performed. Vertebroplasty and kyphoplasty are specific procedures for the treatment of vertebral compression fractures. They are commonly referred to as vertebral augmentation. These procedures can be performed under local anesthesia, sedation, or general anesthesia. A needle is advanced into the fractured bone under X-ray control to establish access.
Both procedures include injection of specific, biocompatible cement material. During vertebroplasty, the cement is directly injected into the bone. Kyphoplasty or balloon kyphoplasty is slightly different from vertebroplasty. During kyphoplasty, a balloon is then inflated inside of the collapsed vertebral body. This way, the vertebral body height and spinal deformity can be restored. Also, cement is delivered into the cavity rather than directly to the bone. The cement hardens within minutes after injection and provides support for the fractured vertebral bone.
Both procedures are very effective in terms of controlling the pain. The choice of the procedure type is up to the treating physician. Since the procedure is minimally invasive, the patients can be discharged on the same day. Therefore, this surgery can be performed for old patients with the poor general condition. Cancer patients also can undergo these surgeries without interrupting chemo- or radiotherapy.