What is the cervical disc herniation?
Cervical disc herniation is a condition characterized by the slippage of the degenerated intervertebral disc into the vertebral canal, causing nerve root and/or spinal cord compression.
What is the structure of the cervical spine?
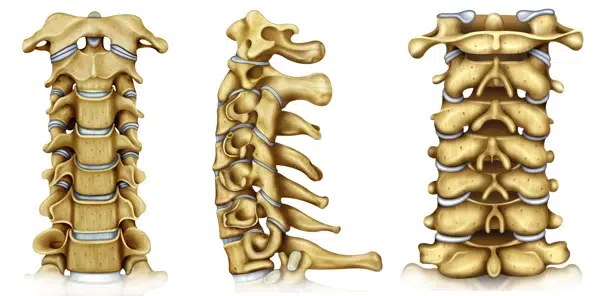
The human head and neck are supported by the cervical spine, which consists of seven vertebral bones and joints between them. The spinal cord passes through the vertebral canal inside the cervical spine. At each vertebra level, the spinal cord gives off a pair of nerves that pass through the intervertebral foramen to exit the spine. These nerves conduct neural impulses between spinal cord and arm.
Each pair of vertebral bones is connected with one big disc joint and two smaller facet joints. The disc joint has a soft, elastic inner core called nucleus pulposus and a tough outer ring – annulus fibrosus. The nucleus is made up of a unique, gel-like substance and serves as an elastic spring between the neighbor vertebra bones. It provides mobility to the spine and serves as a shock absorption buffer. A unique feature of the disc joint is the lack of feeding blood vessels. Unlike other bodily organs intervertebral joints do not have blood flow rather they extract nutricients and oxygen from adjacent vertebral bones. Therefore the survival conditions inside the disc are quite harsh. There is very litte oxygen and nutritions availabe. Only highly specialized chondrocyte like cells can survive in this enviroment. Another distinctive feature of nuclesus is abundance of water, specific type of collagen and proteoglicans. Nucleus holds unique mechanical properties due to these components.
What is disc degeneration and how it leads to cervical disc herniation?
There is continous turnover of disc material. As any mechanical component, disc joint wears off due to mechanical load. Cells inside the nucleus remove waste producte and replace lost parts. There is fine balance betwen wearing off and replacement inside the disc. At some point in life the replacemnt cannot keep up with wearing. As a result, nucleus pulposus loses water, shrinks, and breaks to pieces. This process is called disc degeneration. It is an irreversible process which has no treatment. Fragmented disc pieces break through the annulus fibrosus and slip into the canal. This condition is called cervical disc herniation. Once in the canal, herniated parts compress the spinal cord and nerves. When a cervical nerve root is compromised, the condition is called cervical spondylotic radiculopathy.
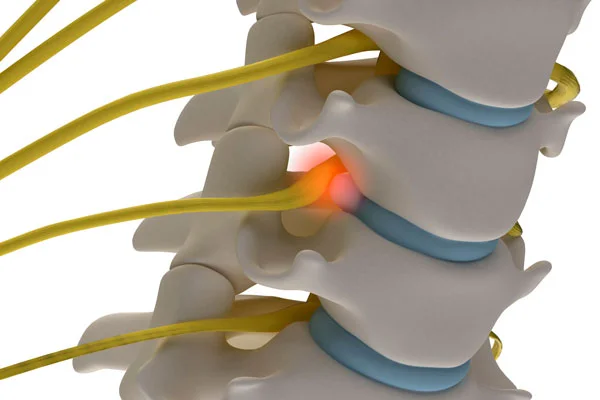
Spinal cord compression is called spondylotic myelopathy. Myelopathy is a more severe condition than radiculopathy and should be promptly treated.
What is cervical stenosis and how it develops?
Degeneration does not always result in cervical disc herniation. In fact, most of the times damaged nucleus slowly wears off without fragmentation and herniation. In other cases, fragmented parts remain inside the disc joint without herniation. With time, the joint collapses under body weight. Such gradual loss of physiological disc height leads to spinal stenosis via several mechanisms.
- Bulging. As noted above healthy nucleus acts like a spring and spreads vertebral bodies apart. This action is necessary to maintain normal disc height. With weakening of the nucleus due to degeneration disc height progressively diminishes resulting in outward bulging of the annulus fibrosus and posterior longitudinal ligament. As a result spinal canal narrows.
- Ligamentous hypertrophy. With loss of nucleus pulpous, adjacent vertebra become slightly unstable. Therefore other supporting structures have to enlarge in order to restore the stability. Ligamentum flavum is one of them and its hypertrophy is a compensatory mechanism for disc degeneration. Unfortunately, ligamentum flavum hypertrophy causes significant narrowing of the spinal canal.
- Loss of intervertebral foraminal height. Degeneration causes disc collapse which brings vertebral bones closer. As a result the height and cross sectional area of intervertebral foramina drastically decreases which leads to spinal nerve root impingement.
- Unco-vertebral joint hypertrophy and deformation. Unco-vertebral joints (UVJ) are paired joints formed by uncinate processes of lower vertebra and corresponding joint surfaces of upper vertebra. Unco-vertebral joints flank disc joint i.e. the disc joint is located between left and right UVJs. With disc height decrease the mechanical load on UVJ increases which in turn results in hypertrophy, osteophyte formation and deformity. Cervical spinal nerve roots pass in the intervertebral foramina just posterior and lateral to the UVJs and may get compressed due to hypertrophy. Extreme hypertrophy may cause bow hunter syndrome due to rotational compression of vertebral artery passing lateral to the uncinate process. In rare cases patients may even develop stroke due to lack of brain blood supply.
- Osteophyte formation. Normally, mechanical load from body weight is evenly distributed through the disc space due to visco-elastic nature of the healthy nucleus. Degeneration leads to uneven load distribution and triggers excessive bone growth. Such extra bone protrusions may narrow either the spinal canal or neural foramina contributing to lumbar stenosis.
- Degenerative spondylolisthesis and retrolisthesis. In some cases, disc degeneration causes loss of vertebral alignment. If supporting ligaments and facet joints cannot compensate for loss of stiffness vertebral bones may lost its normal alignment. Degenerative instability may cause vertebral bone to slip forward (spondylolisthesis or anterolisthesis), backward (retrolisthesis). Such misalignments contribute to stenosis and may compress or stretch nerve roots.
- Kyphosis. Normally, cervical spine has a curve forward which is known as lordosis. The spine generally has alternating forward and backward curves which gives characterizing double S shaped appearance when looking from side. Severe disc degeneration, particularly at multiple levels may affect the shape of the spine. It may manifest as loss of lordosis or worse – kyphosis. In extreme case the neck may get grossly deformed and form swan neck deformity.
What are the symptoms of the cervical disc herniation?

Neck pain
Neck pain is the most common symptom of cervical disc herniation. The pain is mechanical i.e. provoked or made worse by neck movements. Another common feature is cold intolerance. Most patient feel worse during winter and slightly better in summer.
Radiculopathy
Radiculopathy refers to nerve root compression and manifests as neuropathic pain, numbness (hypoesthesia) and weakness (paresis). Every nerve root provides innervation to specific skin area in the arm as well as certain muscles. Therefore every radiculopathy has unique clinical “signature”. Recognizing this pattern and finding out damaged root is clinician’s duty. Usually, radicular pain and numbness are in the same skin are and therefore numbness may not be appreciated. However, patients are usually well aware of weakness (paresis). In advanced cases, muscle wasting (atrophy) may develop.
Myelopathy
Cervical spondylotic myelopathy refers to condition when disc degeneration causes mechanical compression of the spinal cord. It might be acute or chronic. Typical symptoms of myelopathy are numbness, weakness, ataxia (loss of balance), increased reflexes, and urinary incontinence. These symptoms are usually bilateral (present on both sides). Acute myelopathy is usually seen in disc herniation while chronic one is typical for cervical canal stenosis. Due to slow progression of disease patients might not be able to relate their symptoms to disc degeneration especially if pain is not very severe. In some cases with progressive atrophy of the spinal cord patients lose pain sensation which further delays diagnosis. Very frequently they consider symptoms as a part of normal aging and usually seek medical attention when the symptoms are quite severe. Hand muscles’ atrophy is typical in chronic myelopathy.
Sometimes features of chronic myelopathy are not very prominent and patients are unaware of them. In these cases relatively minor trauma may have catastrophic consequences. Cervical stenosis significantly decreases spinal cord’s ability to move inside the canal and even a small impact may cause significant injury. The patients may develop very severe neurological symptoms as a consequence of simple trauma.
Miscellaneous
In rare cases, bone spurs may cause dynamic rotational compression of the vertebral arteries supplying the brain – bow hunter syndrome. These patients suffer from insufficient blood flow to the brain, and the usual symptoms are dizziness, vertigo, and even stroke. Bone spurs may develop in front of the spine, compressing esophagus and patients may have swallowing difficulty (dysphagia).
How is the diagnosis of cervical disc herniation made?
The diagnosis of cervical disc herniation is done by thorough clinical examination and radiological evaluation. Both of them are very important and complement each other. Any discrepancies between clinical and radiological finding should alert the physician and prompt necessary investigation. Failure to do so inevitably results in diagnostic mistakes and treatment fiasco.
Clinical Examination
Proper history and examination is sufficient to suspect the diagnosis. Neurological examination with complete motor and sensory assessment is absolutely necessary since patients might be unaware of their deficits.
History of the disease
History provides valuable clues from very beginning of communication. One of the most consistent features of degenerative cervical disease is mechanical neck pain.
The presence of arm pain is usually the sign of nerve root and/or spinal cord involvement. Neurological deficits especially severe ones, point to compression of the vulnerable neural tissue (either roots or spinal cord) and should alert the clinician.
Clinical Examination
Clinical examination of patients with known or suspected degenerative cervical spine disease should include neurological examination and several specific tests. Neurological examination is basically focused on looking for sensory and motor deficits. As mentioned above, every spinal nerve root provides innervation to specific skin area and muscles in the arm. Therefore careful neurological examination may reveal which nerve root is compromised. Of course the presence and degree of neurological deficit are key factors in formulating the treatment plan. Patients with minimal or no neurological deficits may undergo conservative treatment while significant or rapidly evolving neurological deficits require prompt surgical intervention. Atrophy, increased knee jerk reflexes and ataxia are almost always associated with myelopathy.
One of the most commonly used test for cervical disc herniation is Spurling’s test. During this test a mechanical force is applied to the patient head in tilted position. If pain is induced, the test is positive. The opposite one is the Distraction test. During this test patients head is slightly pulled up. If pain decreases or vanishes the test is positive. Upper Limb Tension Tests are also used clinically for diagnosis of cervical disc disease.
Radiological evaluation
Radiological evaluation is a very important part of assessment. Modern radiological tools can precisely diagnose degenerative cervical disease. They are indispensable for mapping out treatment plan. There are several radiological modalities used for degenerative spine disease diagnosis. Each modality has its own advantages.
MRI

MRI of the cervical spine is the diagnostic test of choice. It gives best resolution of the spine in all three planes. Multiple MRI sequences help to visualize pathology on from various perspectives.
One of the striking advantages of MRI is ability to visualize the disc joint directly. Degenerated discs appear black on T2W images unlike white healthy discs. MRI shows herniation, spinal stenosis ligamentous hypertrophy. Also it helps to differentiate other pathologies like fracture, inflammation, tumor etc.
X-ray
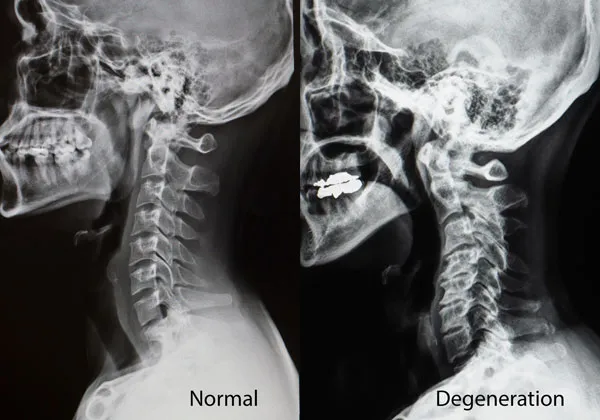
X-rays provide good information about bones, specifically, cervical spine alignment, presence of deformity, bone spurs, narrowing of the disc spaces, vertebral slippage, etc. It cannot visualize soft tissue like disc joint itself or disc herniation. One of the advantages of X-ray that it can be taken while standing and in various conditions like flexing or extending. Such dynamic evaluation might be useful in some selected cases.
CT scan
CT also utilizes X-rays but with much higher resolution. Like X-ray it is suitable for bone visualization. Fractures, misalignments, bone erosions and osteophytes are much better demonstrated by CT scan. It also possible to reconstruct 3D images from raw scan for better visualization.
EMG and nerve conduction studies
EMG, nerve conduction, and evoked potential studies can be performed in some cases to confirm the presence of radiculopathy or myelopathy if the diagnosis is doubtful. However, their practical usefulness is limited. These studies are helpful in distinguishing radiculopathy from peripheral nerve compression syndromes.