Lumbar disc herniation occurs when an intervertebral disc in the lower spine ruptures or bulges outwards, pressing on the spinal nerves and causing pain. Various strategies for treatment are available, which are generally implemented in a stepwise fashion based on the severity of the condition and the effectiveness of previous treatments.
Conservative Management
Conservative treatments are initially preferred for lumbar disc herniations without neurological deficits. Cases with significant deficits like cauda equina syndrome cannot wait and should be treated with surgery. Conservative therapy typically includes pain medication, rest, physical therapy, chiropractic manipulation, and acupuncture. It’s important to understand that these strategies provide symptomatic relief but do not reverse the underlying degenerative process. In order to slow down the speed of degeneration and avoid surgery the damaged disc should unloaded from mechanical compression. Lifestyle modifications like weight loss, smoking cessation, and avoidance of strenuous activities that place significant mechanical load are helpful.
Spinal Injections and Radio-Frequency Ablations
Spinal injections and radio-frequency ablations may be beneficial in some patients. Epidural steroid injections (ESI) can be particularly effective in cases of acute pain though chronic cases are also suitable. Steroids are very potent anti-inflammatory and analgesic medications. They do not eliminate the mechanical compression per se but can resolve inflammation associated with it. The procedure is performed under X-ray control. The doctor guides the tip of the needle to the vicinity of the affected nerve and injects small amount of steroid medication. This way a very high concentration of steroid can be accumulated in around the compromised nerve. Usually depot like medication is used for longer therapeutic effect.
Radio-frequency ablation (RFA) is also used for lumbar disc herniation treatment. Like epidural steroid injection it is performed under fluoroscopic (X-ray) guidance. During RFA procedure a very special needle is used to heat up the tissue. The needle is advanced into the target area under fluoroscopy and then high frequency electrical current is turned on allowing heating of the tip of the needle. The duration and the level of heating depends on the desired effect and the presence of critical structures like nerves. Too much heating of the nerves may irreversible damage them and leave permanent neurological deficits. Usually either facet joints and intervertebral discs are treated with RFA. Heating up destroys tiny nerve branches and relives the pain. However, this procedure cannot treat disc herniation per se or slow down its progression. Therefore the beneficial effect is always temporary.
Surgical Treatment
If conservative measures and less invasive interventions do not provide sufficient relief, surgery becomes suitable choice. Indications for surgery include neurological deficits (such as weakness or sensory loss) or inability to control the pain with non-surgical treatments. The pain should be much enough to compromise quality of life . There are several surgical options for surgical treatment of disc herniation.
Discectomy
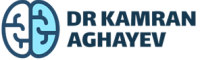
The primary aim of discectomy is to relieve mechanical pressure on the nerves by removing the herniated disc material. There are various forms of discectomy, including open discectomy, micro-discectomy, and endoscopic discectomy.
Open (classic discectomy)
This is the oldest form of discectomy. During surgery the surgeon establishes open access to the involved segment of the spine. Then a small bone window is opened to expose the involved nerve root and disc herniation underneath it. The disc herniation is removed as well as part of the degenerated nucleus pulpous.
Micro-discectomy
All discectomy variations are the same when it comes to the core procedure. However, several modifications exist to lessen the damage to soft tissue covering the spine. The smaller the opening the shorter the postoperative recovery. Micro-discectomy employs surgical microscope which allows excellent illumination and magnification of the area. This way surgical incision may be reduced to a few cm.
Endoscopic discectomy
Like micro-discectomy endoscopic assisted surgery uses a powerful tool for illumination and magnification. Endoscope is inserted directly to the area of disc herniation under fluoroscopic (X-ray) control and then discectomy is performed. The endoscope allows outstanding close up view of the area. Another advantage of the endoscope is minimal or no bone removal. This way damage to the soft tissue envelope and spine itself is minimal.
Lumbar interbody fusion
No matter what type of discectomy is employed long term outcomes are practically the same. The discectomy procedures have a significant drawback – they do not address ongoing disc degeneration . In fact, they accelerate degeneration by inducing surgical trauma to already damaged nucleus. In many cases, disc degeneration accelerates after surgery. Discectomy includes removal of the nucleus pulpous which leads to collapse of the disc space. As a result, intervertebral foramina and spinal canal become narrow leading to nerve root impingement. Such narrowing is called spinal stenosis and it is very frequent after discectomy. Disc joint is pivotal for maintaining stability of the spine. Damage to the disc joint results in loss of stability which provokes pain. Usually the body tries to restore stability by enforcing various spinal ligaments. The strongest one is ligamentum flavum and its hypertrophy is a compensatory mechanism for loss of stability. Unfortunately, ligamentum flavum hypertrophy itself further narrows spinal canal and foramina.
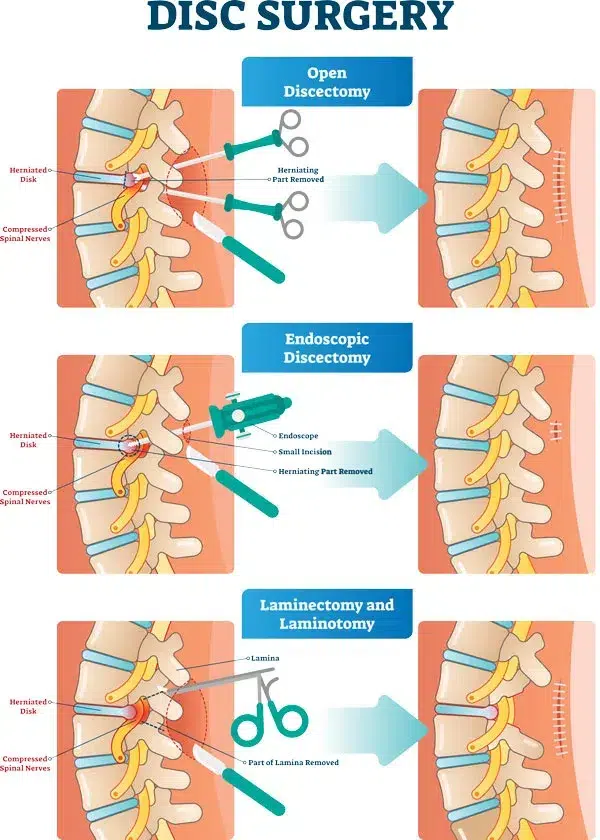
All these factors contribute to failed back syndrome, which is not rare after discectomy. In order to avoid unsatisfactory results many surgeons use spinal interbody fusion procedure. This procedure includes total removal of degenerated nucleus. Therefore, re-herniation is not possible because no disc material is left. After discectomy the empty disc space is filled with bone graft and interbody cage. The cage is a solid device which is inserted into the disc space. It restores normal disc height and widens intervertebral foramina. Bone graft provides biological means for successful fusion of vertebra. Pedicle screws with interconnecting rods are placed to restore the stability and ensure the fusion.
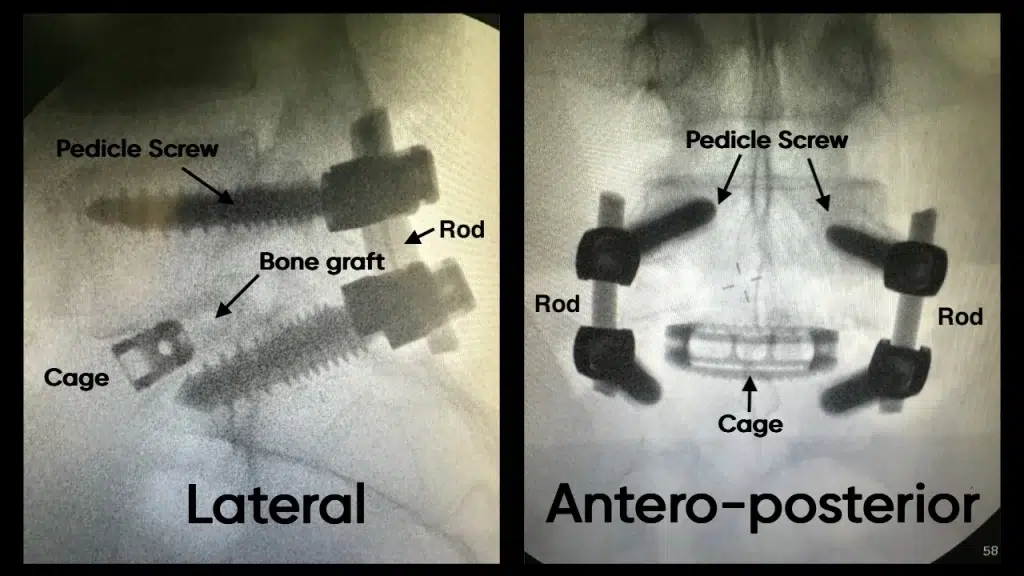
Lumbar interbody fusion has big advantage over discectomy. It treats disc degeneration and therefore there is no chance for post-operative recurrence, spinal stenosis and failed back syndrome. In lumbar spine the transition from discectomy to fusion had been slow, due to technical difficulties. However, nowadays more and more surgeons switch to fusion as primary treatment option.
Recovery and Follow-Up
Recovery from lumbar disc herniation treatments varies greatly depending on the specific intervention and the overall health of the patient. Patients who undergo surgical treatments like discectomy or spinal fusion may need to spend several days in the hospital and may require several weeks to months of rehabilitation. Post-surgical physical therapy maybe used to improve strength and flexibility in the back and to teach proper body mechanics to help prevent future injuries.
Patients should follow up regularly with their healthcare provider to monitor their progress and to detect and address any complications early. Imaging studies like MRI or CT scans may be used to evaluate the treated area.
One of the important aspects of rehabilitation process is lifestyle changes. Eliminating factors that lead to formation of lumbar disc herniation in the first place is essential. In this context, weight loss and smoking cessations are very important. For patients with occupational weight lifting job changing is recommended.
Mental health support, including counseling or support groups, may also be beneficial. Living with chronic pain from a lumbar disc herniation can be challenging, and psychological support can be a valuable part of the recovery process.
In summary, the treatment of lumbar disc herniation involves a combination of lifestyle changes, medication management, physical therapy, spinal injections, and potentially surgery. The choice of treatment depends on the patient’s specific condition, the severity of symptoms, and the response to previous treatments. As with any medical intervention, the risks and benefits should be carefully considered.