Cervical disc herniation is a condition characterized by the rupture and displacement of an intervertebral disc in the neck, which may compress the spinal nerves or spinal cord, resulting in pain and neurological symptoms. The treatment for this condition is typically determined by the severity of symptoms and the effectiveness of various treatment measures.
Conservative Management
Initial treatment for degenerative cervical disc disease and herniation typically begins with conservative approaches. However, some patients have significant compression of the spinal cord and/or nerve roots with severe neurological deficits. These cases should be immediately referred to surgery since attempting to treat them conservatively will waste precious time and may result in catastrophic neurological compromise.
Conservative therapy may include pain medications, chiropractic adjustments, and physical therapy. In some instances, local steroid injections or radio-frequency ablation may be recommended to provide more targeted relief.
Epidural Steroid Injections
Epidural steroid injections (ESI) are less useful in cervical spine in comparison with lumbar segment. The main reason is technical. In the cervical area there a several critical structures around and within the spine which make the procedure difficult and risky. The procedure is performed under X-ray image guidance. The needle is placed so that the tip is close to the affected nerve. Steroid solution with local anesthetic is injected which provides analgesic and anti-inflammatory effects. ESI do not treat the disc degeneration nor mechanical compression per se, that is why their effect is temporary. In some cases though steroid injections provide long lasting effect. This effect is not due to injection but to natural course of the disease.
Radio-Frequency Ablations (RFA)
This procedure aims to heat up the tissue in the involved area and relieve pain by damaging tiny nerves responsible for pain conduction. RFA needle can placed into or around the facet joint or into the disc joint under X-ray control. Once high frequency electricity is turned on the tip of the needle heats up causing thermal damage. The duration and intensity of heating varies depending on the desired effect. Like ESI radio-frequency ablation mitigates the pain and doesn’t treat the disease, therefore the effect is temporary.
Surgical Treatment
Indications
There are two indications for surgical treatment when it comes to cervical disc herniation. Patients with severe neurological deficits should have surgery as soon as possible to prevent irreversible damage. Spinal cord and nerves cannot handle significant mechanical pressure for a long time. If compression is not lifted neurons and their delicate fibers (axons) quickly die. The nervous system cannot replace lost neurons due to its limited regenerative capacity. Therefore any patient with neurological injury is a candidate for surgery. This is particularly true for patients with severe or worsening symptoms. Delaying surgery in these patients may result in permanent deficits. The second indication for surgery is failed conservative treatment. As discussed above patients with minimal or absent neurological symptoms are treated with non-surgical methods. Generally conservative treatments are effective in reducing the pain in short term. Long term results aren’t much encouraging because conservative treatment doesn’t affect natural course of disc degeneration. When pain continues despite conservative therapies the surgery comes to consideration.
Overview of Surgical Techniques
There are several alternative surgical options used for cervical disc herniation. The main goal is to remove compression from the nerves and spinal cord and restore normal function. The surgery can be performed either from the front (anterior approach) or the back (posterior approach) of the neck, based on the patient’s condition and the surgeon’s preference. The second surgical goal is to deal with disc degeneration itself. In this perspective there are two options – fusion or cervical disc prosthesis.
Anterior cervical discectomy and fusion (ACDF)
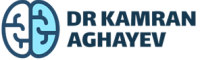
It is the most commonly used surgical procedure for cervical disc herniation. The surgery is performed from the front of the neck (anterior). The surgeon exposes the cervical spine by carefully passing between delicate neck organs like carotid artery, esophagus etc. He might use fluoroscopy (X-ray) to verify the correct disc joint. Once the correct disc is confirmed the surgeon removes the damaged disc joint. This part includes total removal of degenerated nucleus pulpous and all slipped disc fragments. If there are hard bone spurs causing impingement they are removed by bone cutting tools. Once the source of compression has been eliminated, the neighboring disc joints are merged together to provide stability. First the empty space left after disc joint removal is filled with a an interbody cage. The cage is ring-like implant filled with bone graft to facilitate the fusion. The main function of the cage is to restore and maintain optimal distance between the vertebral bones. This distance should be close to natural disc height. Very frequently degeneration causes disc collapse and nerve root impingement in the intervertebral foramina. Restoring the normal height is called indirect decompression and is very important part of the procedure. The cage is filled with bone graft which helps to develop solid bone bridge and fuse vertebral bones together. The quantity and the quality of the bone graft is of paramount importance. The best choice is patient’s own bone which is called autograft. Usually this bone is harvested from the iliac bone via small incision. The interbody cage is filled with the bone graft and inserted into the disc space. Usually fluoroscopy (X-ray) is used to confirm the position of the cage. Titanium plate and screws can be used to fix the vertebra together and facilitate fusion.
Although the procedure is called anterior cervical discectomy and fusion it is slightly misleading name. The fusion doesn’t happen during surgery. The procedure is performed with intention for fusion. Fusion is a biological process and involves new bone formation. A newly formed bridge links adjacent bones together and the process takes several weeks or moths. This process is analogous to fracture healing when newly formed bone unifies broken fragments. Of course, significant part of success comes from expert surgical technique i.e. properly positioned cage filled with high quality bone graft in combination with plate and screws.
ACDF is highly successful procedure and that is the main reason why it is extensively used for cervical disc herniation treatment. The rate of successful fusion and patient satisfaction is very high. The main problem with ACDF is fusion itself. When disc joint is fixed the its functions shifts to adjacent joints which have to take extra motion to maintain motion. The increased load may damage the discs and accelerate the degeneration. This phenomenon is known as adjacent segment disease.
Posterior Cervical Discectomy
This procedure is rarely performed nowadays. The surgeon approaches the injured site from the back. After approaching the spine the compressed nerve root is exposed from a small bone window. The nerve is gently moved and disc herniation is removed. This technique is analogous to lumbar discectomy.
There are several shortcomings associated with this technique. First, it does not address the disc degeneration itself. Second, midline and paramedian (near midline) herniations compressing the spinal cord cannot be safely reached via this route.
Posterior Laminectomy with or without Fusion
This type of surgery is usually used for cervical canal stenosis treatment. The surgeon exposes the spine from the back (posterior) and then removes vertebral lamina to widen the spinal canal. Alternatively, some surgeons do not remove the lamina, rather cut, rotate and re-stabilize them via small plates and screw. This technique is called open door laminaplasty or simply laminaplasty.
Cervical laminectomy has several drawbacks. Firstly, lamina are essential for maintaining normal shape of the cervical spine and removing them may result in kyphotic deformity. This condition is called post-laminectomy syndrome. To avoid post laminectomy syndrome surgeons frequently use posterior cervical screw stabilization. However, posterior stabilization doesn’t yield good fusion. Secondly, the posterior surgery does not address disc degeneration. Cervical disc degeneration and cervical stenosis are consequences of cervical disc degeneration. Any surgery trying to address the secondary problem without fixing the primary issue is doomed to fail. Besides the majority of compression in degenerative disc disease comes from anterior and cannot be addressed via posterior route. Thirdly, degeneration usually causes nerve impingement due to disc height collapse. Unlike ACDF, posterior surgery cannot restore normal disc height and provide indirect decompression.
Cervical Disc Prosthesis
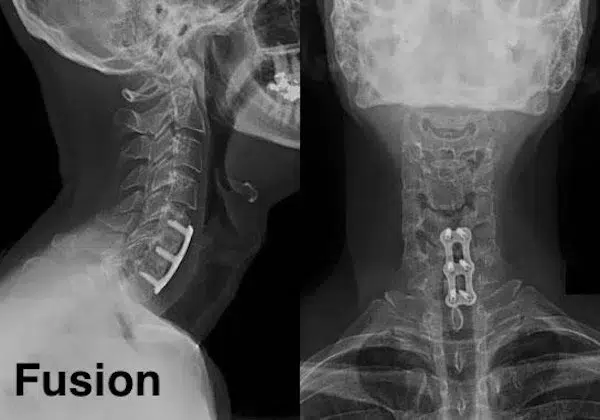
As discussed above anterior cervical discectomy and fusion restricts normal motion and may result in adjacent disc disease. To mitigate this problem a novel technology has emerged. Cervical disc prosthesis is an alternative technique aiming to preserve and restore motion. An artificial joint is inserted as substitute for the removed disc joint. This technique allows for the preservation of motion at the surgical site, which can be beneficial because it reduces additional load on the adjacent joints. As a result, the likelihood of developing disc degeneration may be lower compared to fusion.

Cervical disc prosthesis is an excellent idea in theory. Practically, there are several issues with artificial spinal joints. Currently there are no materials to mimic normal disc function. Various metal and plastic combinations are used but none of them even close to healthy discs. The idea of artificial spinal joints was conceived in 1980’s and multiple companies came with various products. Unfortunately, none of them passed time test and eventually were withdrawn from the market. Today there are a handful of companies making artificial cervical disc prosthesis. But these devices hit the market relatively recently and chances are they will be abandoned in future like their predecessors. Previous experience with cervical disc prosthesis shows that frequently they either fuse or deform cervical spine. Fusion however is much better because once successfully fused vertebra will stay in that position for the rest of life.
Recovery and Follow-Up
The recovery process from cervical disc herniation treatments vary based on the intervention and the overall health status of the patient.
Patients who undergo surgical interventions, such as ACDF may need to stay in the hospital for a few days. To ensure solid fusion the patients should pay attention to their overall health. In this context adequate vitamin D levels and smoking cessation deserve special attention. Vitamin D is very important for new bone formation (as well as maintaining healthy bone) and its deficiency may result in poor fusion. Therefore patients are encouraged to take vitamin D supplements and maintain adequate blood levels for successful outcomes. Smoking is a significant healthcare issue. It impedes with fusion process and may result is poor outcomes. Therefore, patients considering cervical fusion should quit smoking prior to surgery.
Mental health support, including counseling or support groups, can also play a crucial role in the recovery process. Chronic pain from a cervical disc herniation can pose psychological challenges, making emotional support an integral part of recovery.
In conclusion, the treatment of cervical disc herniation involves a combination of conservative measures, injections, and potentially surgery. The specific treatment approach depends on the patient’s symptoms, the severity of the condition, and their response to previous treatments. All treatment options come with their own set of risks and benefits, which should be carefully considered.