How do we diagnose TOS?
The diagnosis of thoracic outlet syndrome is difficult because there is no universal confirmatory test. An important part of diagnosis comes from recognizing TOS as a possible cause of the patient’s problems. Even experienced doctors may not recognize the signs and symptoms of TOS. For example, a study in the United States found that patients visited an average of four doctors before receiving an accurate diagnosis.1. However, if thoracic outlet syndrome is suspected, the diagnosis is actually more likely to be accurate. According to a large-scale referral center study in the United States, the accurate diagnosis rate for physician referrals was 91% and for patient self-reports was 97%.2. This study shows that patients diagnose TOS as well as their doctors.
Suspecting TOS is the first step, but many tests must be performed to confirm the diagnosis. Because the causes of TOS are varied, diagnosis requires careful evaluation. Furthermore, different causes require different tests to identify them. Diagnosing TOS is like putting the pieces of a puzzle together. An experienced doctor can see what others miss and recognize TOS at even the slightest signs. Therefore, physicians must be patient, attentive, and skilled in clinical examination and radiological imaging.
Clinical evaluation
History
A careful history and physical examination are important keys to suspecting thoracic outlet syndrome. TOS is a chronic condition and patents report long-lasting symptoms. Certain symptoms, such as pain on exercise or inability to perform additional tasks, require special attention. These tips can indicate the presence of TOS right from the start of the evaluation. After speaking with numerous TOS sufferers, I discovered that there is a specific “TOS pattern”. Recognition of this pattern is conscious and intuitive to the practitioner.
Physical examination
Poor posture carries risk for TOS development and I always check postural abnormalities. Kyphosis, scoliosis, shoulder and collar bone asymmetry are frequent in TOS patients. They are usually subtle and barely visible to untrained eye and therefore frequently missed. Pain and tenderness at the junction of the neck and shoulder area is very typical but not specific to TOS. Tapping of the thoracic outlet area from behind usually triggers pain and is my preferable test because it is highly sensitive to TOS.
Neurological assessment
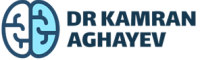
The neurological examination should focus on muscle weakness and sensory disturbances in the arms and hands. Proper examination and interpretation of results requires a thorough knowledge of the anatomy, branches, and skin/muscle distribution of the brachial plexus.
Motor (muscle strength) examination
This part of the neurological exam should focus on muscle atrophy (wasting) and muscle weakness.
Atrophy
Muscle wasting is particularly important because it is an indicator of the severity of the disease. Atrophy is usually prominent on thenar (lateral) side of the hand. I check the atrophy by comparing two hands side by side. This way even subtle muscle wasting is visible. The presence of atrophy is a “red flag” because it indicates that the problem has been going on for a long time and is starting to have lasting effects.
Muscle weakness
All hand muscles receive innervation from the lower part of brachial plexus – specifically by C8 and T1 nerve roots. Usually all hand muscles weak on testing. This clinical finding distinguishes TOS from other nerve entrapments like carpal tunnel or cubital tunnel syndromes. In carpal tunnel syndrome the hypertrophic (enlarged) transverse carpal ligament compresses the median nerve in the wrist. Some (but not all) hand muscles get weak as result of nerve smashing. These are LOAF muscles – L: lateral two lumbricals, O: opponens pollicis, A: abductor pollicis brevis, F: flexor pollicis brevis. In cubital canal syndrome all other hand muscles are affected. Significant number of TOS patients get wrong diagnosis of carpal or cubital tunnel syndrome and even have unnecessary surgery.
Sensory (skin feeling) examination
Neurogenic TOS causes variety of sensory disturbances. They include pain, paresthesia (pins and needles), numbness in the affected area. Correct sensory examination can significantly contribute to TOS diagnosis. Alas this is rarely done for several reasons. Firstly, thorough sensory examination of entire arm for all sensory modalities (touch, pain, temperature, vibration) is time consuming. Rather small areas are superficially examined to speed things up. Secondly, most physicians do not have deep knowledge regarding complex anatomy of arm innervation.
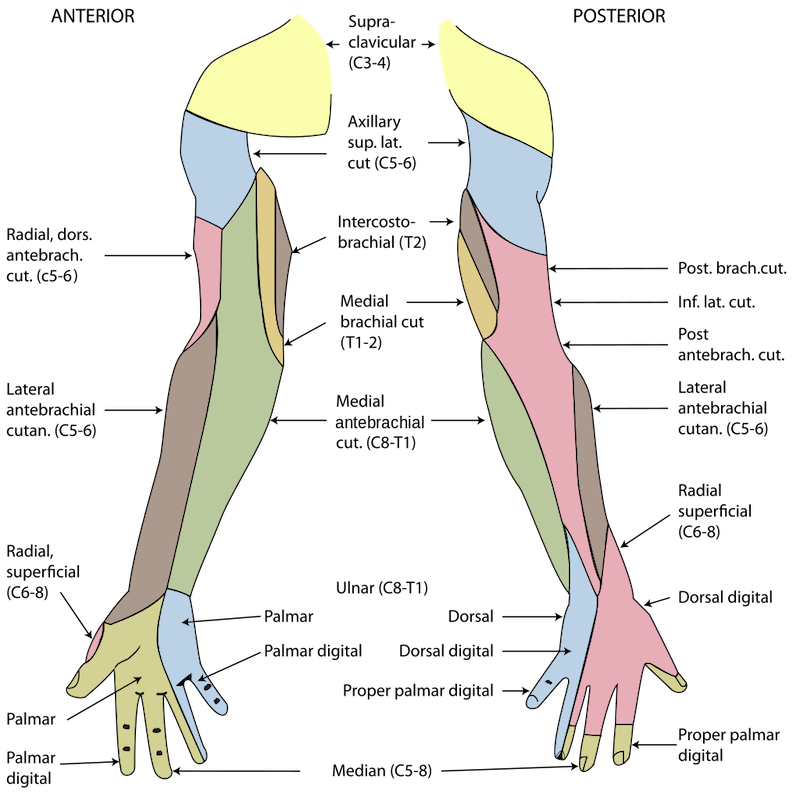
In my experience, most doctors confuse thoracic outlet syndrome with ulnar nerve entrapment. The lower part of brachial plexus comprises C8, T1 roots which join together to form the inferior trunk. This part of the brachial plexus is most vulnerable to compression and most frequently affected by TOS. Inferior trunk gives off several branches which eventually innervate the skin of the inner (ulnar) side of the arm, forearm and hand. Therefore, sensory problems in this area are specific for TOS. The common mistake done by doctors is to attribute inner forearm hypesthesia to ulnar nerve entrapment. The ulnar nerve has no sensory innervation in forearm. In other words, affected sensory area in TOS includes ulnar nerve area but not restricted to it. The skin of the inner side of the arm and forearm receive innervation from other nerves – intercostobrachialis and medial cutaneous antebrachial nerves. As mentioned above neurogenic TOS affects mostly C8/T1/inferior trunk and its branches – ulnar, medial cutaneus antebrachial, intercostobrachial. From all these nerves medial cutaneous antebrachial nerve has the highest diagnostic value and its involvement is very specific for TOS. Yet its skin area is rarely examined and if examined hypesthesia is wrongly attributed to ulnar nerve compression.
Provocative maneuvers
Provocative testing is an essential part of clinical examination. The purpose of these tests is to trigger TOS symptoms using specific clinical maneuvers in order to establish diagnosis.
- Elevated arm stress test (EAST or Roos test). It is most commonly used and most informative test for diagnosing TOS. Arms are abducted and elevated and the patient opens and closes his hands. The presence of fatigue, pain and numbness is an indicator of thoracic outlet syndrome.
- Upper limb tension tests (ULTTs). These are several tests aimed to evaluate various nerves of the arm. One of them is performed with arms abducted, palms dorsiflexed and head is tilted. If pain is experienced the test is considered positive.
- Adson’s test is frequently used to diagnose arterial compression. However this test is highly misleading and has practically no value. Adson’s test seeks for subclavian artery compression and disappearance of radial pulse as a proof of TOS syndrome in certain position. This test lacks specificity and sensitivity because it is positive in many normal individuals and frequently negative in TOS patients.
Radiological examination
X-ray
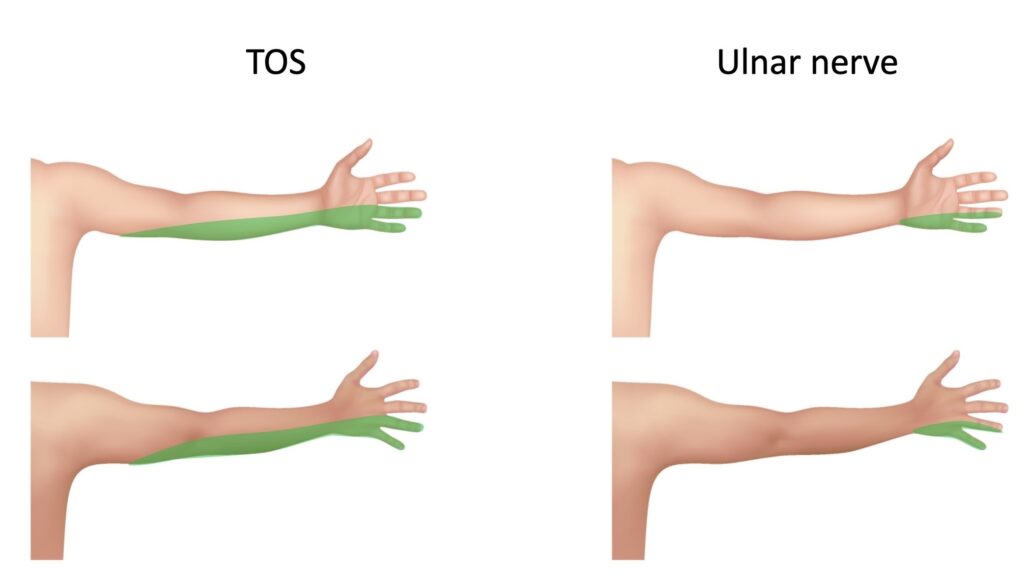
This is a very useful tool for diagnosing simple bone abnormalities. For example, accessory cervical ribs are visible on X-rays. Sometimes, though these ribs may be in the form of long C7 transverse processes which will make diagnosis more obscure. Other anomalies like poorly healed first rib and clavicle fractures, abnormal and mispositioned bones are difficult to see on X-rays. X-rays are also helpful for distinguishing TOS from advanced cervical disc disease. Very often patients with neurogenic TOS have loss of lordosis (neck straightening) or even cervical kyphosis which is incorrectly attributed to cervical disc herniation. In fact loss of lordosis is very common in TOS . The main disadvantage of X-ray imaging is ionizing radiation.

CT scan
This is an outstanding tool for in-deep bone scanning. Soft tissue can also be shown but to lesser degree. CT angiography (CTA) is perfect for subclavian artery and vein visualization. Three-dimensional CT/CTA reconstructions can be particularly helpful for preoperative assessment. Combined with provocative arm positioning to accentuate compression, CT/CTA demonstrate the site and cause of compression with high precision. The main disadvantage of CT scan is ionizing radiation.
Ultrasonography (USG) and Duplex scan
USG has been used in medicine for decades. But it was relatively recently when ultrasonography was implemented in TOS. High-resolution USG of the thoracic outlet area can directly demonstrate the neuro-vascular bundle compression. Doppler ultrasonography or Duplex scan is a variant of USG and shows the blood flow. It is particularly useful in arterial and venous TOS cases. One of the biggest advantages of USG is its “real time” feature. This means that the imaging is very fast and reflects the current state. This feature allows scanning in normal and provocative positions, for example with arms abducted at various angles. USG is free from ionizing radiation and is the safest imaging modality. It is relatively inexpensive as well. The main disadvantage of USG is subjectivity. It means that results depend on a person performing the scan.
MRI
It is the most effective tool to demonstrate the soft tissue. Compared with other imaging options MRI has the highest resolution quality. It can differentiate TOS from cervical disc disease. Standard MRI in neutral position is not very useful. However provocative imaging with arms above the head is the best imaging modality for TOS. The clavicle moves closer to the first rib in this position resulting in “nutcracker effect” resulting in neuro-vascular compression. MRI can visualize this compression directly. In addition to standard and provocative imaging there are many different MRI protocols. For example, MRI neurography visualizes the brachial plexus itself with high accuracy. Diffusion tensor imaging (DTI) shows fiber orientation inside the brachial plexus. MR angiography or MRA can show blood flow in subclavian vessels. MRI is very safe because it is not based on ionizing radiation. The disadvantages of MRI are long scan time and expensiveness.

Electromyography (EMG) and Nerve conduction studies
Many specialists consider electromyography (EMG) and electroneurography (ENG, nerve conduction studies) as an essential part of thoracic outlet syndrome diagnosis. In theory it is very logical. TOS affects brachial plexus nerves and EMG should be able to detect the damage. However in practice the situation is much complex. There are several reasons why EMG fails to diagnose TOS.
- Nerve conduction studies measure various parameters of nerve conduction (speed, amplitude, latency etc) across specific area. The area where the nerves are close to skin are easy for testing. Therefore, entrapment neuropathies like carpal tunnel and cubital canal syndromes are easily diagnosed because the nerves are superficial. Brachial plexus is very deep and cannot be evaluated directly.
- Nerve conduction is usually measured by placing probes proximal and distal to the affected area. The brachial plexus is too close to the spinal cord and proximal probe cannot be placed.
- The nature of compression is intermittent i.e., occurs when arm is up. Thus standard EMG (arms down) cannot show the compression.
- The normal values for EMG and ENG are too variable and the results mainly depend on the specialist making the test very unreliable.
The sensitivity of EMG for TOS has been studied in a recent meta-analysis study. This study conducted in depth analysis of all studies regarding EMG and came to conclusion that “Electroneuromyography cannot be considered a true diagnosis tool for NTOS at this point”.3. However, several studies showed that specific EMG tests like medial cutaneous antebrachial nerve EMG has value in TOS patients. However, these tests are not part of standard EMG and rarely performed. Therefore, from practical point of view EMG nowadays is useless test.
There is a big problem with EMG though. As we discussed, it has very little value in detecting TOS but doctors traditionally rely on it. Historically when imaging modalities were not avialable physicians used EMG for diagnosis. Even then, back in 1970s prominent TOS experts criticized it4. Today, false negative EMG results are used as justification to rule out thoracic outlet syndrome. This is the main reason why patients cannot find adequate treatment for their condition and suffer for many years.
Next: Standard Thoracic Outlet Syndrome Surgery
References
- Landry GJ, Moneta GL, Taylor LM, Jr., Edwards JM, Porter JM. Long-term functional outcome of neurogenic thoracic outlet syndrome in surgically and conservatively treated patients. J Vasc Surg. 2001;33(2):312-317; discussion 317-319. https://doi.org/10.1067/mva.2001.112950 [↩]
- Likes K, Rochlin DH, Salditch Q, et al. Diagnostic accuracy of physician and self-referred patients for thoracic outlet syndrome is excellent. Ann Vasc Surg. 2014;28(5):1100-1105. https://doi.org/10.1016/j.avsg.2013.12.011 [↩]
- Daley P, Pomares G, Gross R, et al. Use of Electroneuromyography in the Diagnosis of Neurogenic Thoracic Outlet Syndrome: A Systematic Review and Meta-Analysis. J Clin Med. 2022;11(17). https://doi.org/10.3390%2Fjcm11175206 [↩]
- Roos DB. Congenital anomalies associated with thoracic outlet syndrome. Anatomy, symptoms, diagnosis, and treatment. Am J Surg. 1976;132(6): 771-778. https://doi.org/10.1016/0002-9610(76)90456-6. [↩]