In this article, we’ll discuss conservative and surgical hemifacial spasm treatment options, including medications, Botox, and microvascular decompression for facial hemispasm.
Living with hemifacial spasm
Hemifacial spasm (AKA tic convulsif) is a neurosurgical disorder, characterized by involuntary contractions of facial muscles occurring usually on one side of the face.
Social and psychological issues in hemifacial spasm
It is a challenging condition to live with because facial expressions are essential for human communications and we constantly focus on faces. People are genetically programmed to concentrate on others faces particularly during social interaction. Abnormal, uncontrolled twitches on the patient’s face give impression that something strange is going on. Most people are unfamiliar with hemifacial spasm and it is very hard for them not to look to these spasms. Often they cannot hide perplexity or stupefaction. Patients are very well aware of people’s reactions and feel deeply embarrassed. As a result they diminish social interactions – especially with unfamiliar people. Frequently patients become socially withdrawn, depressed and develop suicidal ideas.
Physical signs in hemifacial spasm
Besides muscle contractions hemifacial spasm may cause several physical signs. Persistent contractions of periorbital muscles cause prolonged eye closure and may lead to functional blindness. Decreased vision significantly lowers patients’ quality of life. In addition to functional blindness patients may develop lacrimation issues such as dry eye. Hemifacial spasm is caused by focal demyelination of the facial nerve at the brainstem level. Parasympathetic fibers responsible for normal lacrimation are passing inside the facial nerve and may be damaged by neuro-vascular conflict. This damage is the main mechanism leading to dry eye syndrome which may cause corneal damage and lead to permanent visual loss. Hearing problems are frequent in hemifacial spasm and may include hypoacusis (decreased hearing), ear clicks and tinnitus. Acoustic symptoms arise from stapedius muscle spasms, VIII nerve irritation or Eustachian tube disfunction.
Hemifacial spasm treatment
It is usually said that there are there options for hemifacial treatment i.e., medical treatment, facial Botox injections and surgical microvascular decompression. However, one should always remember that these aren’t really options. When it comes to cure the only option is surgery. Medical treatment and Botox injections do not treat the disease itself.
Drug therapy for hemifacial spasm
There are several medications used for HFS “treatment”. Drugs like carbamazepine, clonazepam, gabapentin are frequently prescribed for patients with hemifacial spasm. All of them are epilepsy medications and presumably work by interfering with abnormal impulse generation in the facial nerve root entry exit area. However, clinical benefit is not very impressive to say the least. Besides they do not treat the cause of disease and patients take these drugs for entire life. Due to prolonged usage, side effects are not infrequent. Some of them like hyponatremia or Stevens-Johnson syndrome are life threatening.
Botox injections
Facial Botulinum toxin or simply Botox injections are frequently used for hemifacial spasm treatment. It is basically a poison, obtained from bacterium Clostridium botulinum and interferes with transmission of signals from nerves to muscles, inducing muscle paralysis. This interference is indiscriminate i.e. both normal and abnormal impulses are blocked at neuro-muscular junction. As a result of Botox induced paralysis the muscle becomes unresponsive to nerve signals and therefore twitching subsides. There are two major problems with Botox injection in hemifacial spasm.
Temporary effect of Botox injections
Botox treatment does not cure the hemifacial spasm i.e. does not interfere with abnormal impulse formation in the facial nerve. The demyelinated area in the REEZ zone keeps generating aberrant signals as before. Therefore, once the effect of Botox subside facial contractions recur. Botox effect lasts approximately 2-3 months and usually by the end of this period facial twitching is back.
Facial palsy due to repeated Botox injections
As discussed above Botox injections do not permanently treat the hemifacial spasms. Therefore, patients keep getting more shots. A muscle paralyzed by Botox usually receives within 2-3 months. However, the muscle never regains its original strength. There is always permanent small permanent muscle palsy after each Botox injection. This effect is negligible for a single injection but may be quite significant after repeated shots. Very frequently patients end up with iatrogenic (treatment induced) facial palsy. On top of that the remaining weak facial muscles keep on twitching. Sometimes patients undergo so many injections that most of their facial muscles disappear and the patients end up with disfiguring facial palsy.
Microvascular Decompression (MVD) for hemifacial spasm
Microvascular decompression (MVD) is the only permanent treatment for patients suffering from hemifacial spasm. The aim of surgery is to eliminate the source of abnormal impulses in the facial nerve. The procedure consists of two stages – access and microvascular decompression itself.
The approach
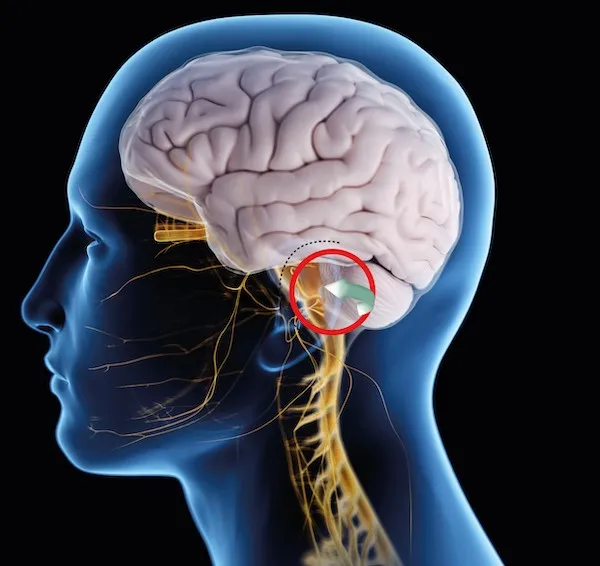
The approach to the facial nerve area is called retrosigmoid because the working corridor is behind the sigmoid sinus. A small incision is made behind the ear and soft tissue is stripped away from the skull to expose the bone. Then a small bone window is opened just back to the sigmoid sinus. Bone opening exposes dura mater which is the cover for the brain. The dura is cut and then neurosurgeon proceeds further deep in to the brain. Usually, either surgical microscope or endoscope is used at this stage. Both of them allow magnification and illumination of the deep tiny area of the facial nerve. In order to access the facial nerve the surgeon must work between the skull and the cerebellum. The best way is to drain cerebrospinal fluid allow the brain to sink. This way a natural corridor between the brain and skull opens up and surgeon proceeds effortlessly.
The decompression
The facial nerve is easy to find due to shallowness and consistent position. Surgeon must cut arachnoid membranes surrounding the nerve to fully expose it and expose the offending vessel. Needless to say that this and subsequent steps require superb microsurgical skills and expertise.
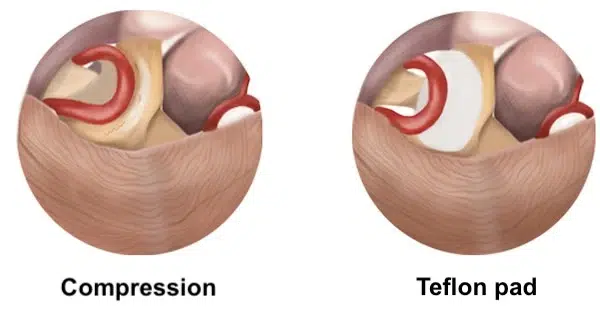
The objective of MVD is to identify, separate and isolate the blood vessel(s) compressing the facial nerve. Usually the vessel is stuck to the nerve by tiny arachnoid fibers. Also the vessel itself has arachnoid membranes holding it. Basically the arachnoid membranes are everywhere – around the nerve, artery and in between them. These membranes are cut until the vessel is free from the nerve and can be moved away easily.
There are two surgical techniques used for microvascular decompression – interposition of transposition. Interposition is an older one and includes inserting something between the facial nerve and offending vessel. Usually tiny pieces of teflon felt are used. They keep the artery away from the nerve and eliminate pulsatile pressure. Alternatively a piece of muscle or fat can be used. Another technique is transposition when the artery is moved away and fixed so there is no physical contact with the nerve. Transposition is technically more difficult and might not always feasible. For example if the compressing vessel travels between the 7th and 8th nerve it is not possible to move the vessel away from the facial nerve without compromising the vestibulo-cochlear nerve. In these cases the interposition is the only choice.
After decompression the surgeon closes the dura by suturing then puts as small cover over the bone window. The muscles and the skin are also sutured.
The facial and vestibulo-cochlear nerves are very fragile and surgical manipulation may inadvertently hurt them. Therefore some surgeons may use intraoperative EMG and brainstem auditory evoked potential monitoring during the procedure to prevent the damage. It goes without saying that the most important factor affecting the outcome is surgeon’s experience and skills. Some surgeons may not need sophisticated tools and give excellent results. Generally, MVD is a highly successful procedure, providing a complete cure in approximately 85-90% of cases.
Recovery after microvascular decompression
The recovery period following MVD surgery is usually swift, but it’s important to note that symptoms may not disappear immediately post-procedure. In some instances, several weeks or months are required before noticeable improvement is observed. It is due to the fact that ectopic area inside the facial nerve may not cool down immediately after the procedure. The patients must know that the goal of surgery is eliminate the compression. Demyelinated area developed at the of neuro-vascular conflict zone needs some time for regrowing myelin. This is a cellular process and time for remyelination varies from patient to patient. According to the literature full benefit of surgery may take up to 800 days to occur.
Post-surgery, patients can expect some discomfort at the site of the incision, which can be managed effectively with pain medication. Depending on the patient’s overall health and the extent of the surgery, a brief hospital stay of a few days is typically required.
Recovery is a gradual process and patients are encouraged to slowly return to their regular activities, as comfort allows. Regular follow-up appointments with the neurosurgeon are vital to monitor the healing process and to check for potential complications.
Complications of microvascular decompression
There are two types of complications associated with MVD surgery – complications of due to access and specific complications of microvascular decompression surgery. Access complications include cerebrospinal fluid leak, surgical site infection, poor healing, chemical meningitis. Their occurrence is not different from other brain surgeries and usually they are quite rare. Specific complications include facial nerve and vestibulo-cochlear nerve damages. These complications are believed to arise from surgical manipulation and in most cases temporary. Some surgeons may use intraoperative monitoring to decrease the rate of these complications.
