What is the brain aneurysm?
A brain aneurysm is a condition characterized by ballooning and expansion of the brain vessel’s wall, which can potentially rupture and cause bleeding.
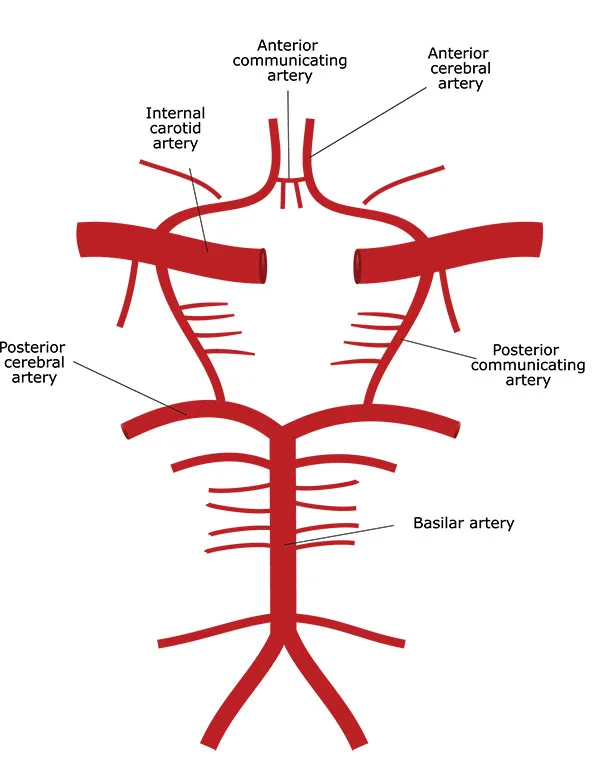
How does the brain get its blood supply?
The brain is a very energy-consuming organ. It weighs around 1.5 kg yet takes approximately 15% of total blood flow and 20% of total oxygen consumption. It is supplied by four major vessels – two carotid and two vertebral arteries. These arteries form a complex network called The Circle of Willis, which supplies the brain by giving off smaller branches. The Circle of Willis allows the brain to maintain blood flow in cases of major artery obstruction. It is an evolutional adaptation to keep all brain parts continuously supplied. Technically, brain arteries and circles of Willis are located outside of the brain in the subarachnoid space. This space is filled with cerebrospinal fluid.
Why do the brain arteries develop aneurysms?
The flow and the pressure in the brain arteries are very high due to massive demand. Also, the wall of brain arteries lacks an external supporting layer (tunica externa or adventitia layer) present in other arteries. Therefore, brain arteries are very prone to aneurysm formation. The weak spots in the artery wall become bulged due to pressure inside of the artery. These small bulges are sometimes called blister aneurysms because they can also rupture and cause bleeding. With time, this bulge became more and more prominent due to the Laplace law. According to this law, the greater the diameter of the vessel, the greater the tension of its wall, given the pressure is constant. Therefore, bigger aneurysms tend to rupture more frequently.
All brain aneurysms are true aneurysms, unlike false aneurysms that may develop in other areas. Brain aneurysms usually develop at sites where the artery branches off.
Blood flow at branching sites is usually turbulent, putting additional mechanical stress on the arterial wall. Thus, these sites are especially prone to aneurysm formation. High blood pressure (hypertension), smoking, genetic predisposition (familial cases), and atherosclerosis are factors contributing to aneurysm formation.
How many brain aneurysm types are there?

There are three types of brain aneurysms:
Berry or saccular aneurysms – the most common type of aneurysms. These aneurysms develop due to dilation of the part of the artery wall. They usually have rounded shape and may be from several millimeters to several centimeters.
Usually, these aneurysms become symptomatic due to rupture or compression of nearby structures. They may also develop due to increased flow and turbulence. If one of the main brain arteries is occluded, the others have to compensate through the circle of Willis. Increased flow puts additional mechanical stress on arteries, leading to aneurysm formation.
Brain arteriovenous malformations (AVM) are also frequently associated with aneurysms. AVMs divert blood flow from the brain tissue directly to veins. Since this alternative way has very low resistance, the flow is very high. Therefore, aneurysms often develop on arteries supplying AVM and on the circle of Willis.
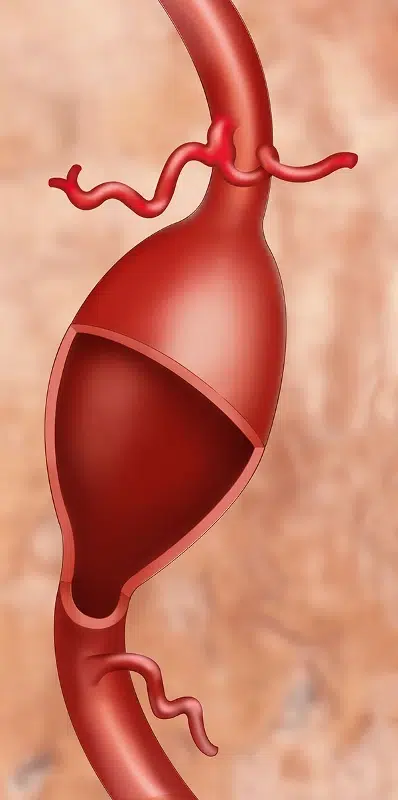
Fusiform aneurysms – these aneurysms are dilation of the entire wall of the vessel and resemble a spindle. They also have the potential to rupture, but in the vast majority of cases, they usually cause compression of nearby structures and cause neurological deficits. In some instances, the flow in the aneurysm is slow due to dilation, which leads to blood flow stagnation and thrombus formation. These thrombi may dislodge and cause blood flow obstruction, leading to ischemic stroke.
Mycotic aneurysms – these aneurysms form due to infection. They are usually associated with infective endocarditis. Infected thrombi with bacteria in it may get stuck inside brain vessels. Bacteria will cause inflammation inside the artery wall, leading to weakening and aneurysm formation. These aneurysms usually develop on small brain arteries and are very rare.
What are the symptoms of a brain aneurysm?
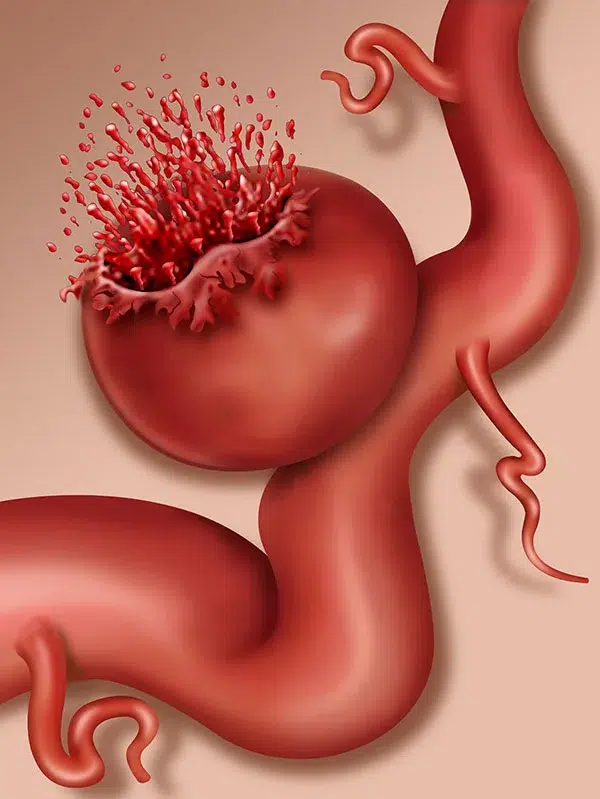
In the vast majority of cases, brain aneurysms do not cause any symptoms until they rupture and cause hemorrhage. Since brain arteries are located in the subarachnoid space, blood spills into this space, causing a subarachnoid hemorrhage.
This type of hemorrhage is associated with the sudden onset of severe headache. Some patients refer to it as the worst pain of their life. This pain is due to irritation of the meninges (brain covers that are very rich with pain receptors).
Blood spilled into the subarachnoid space forms clots within minutes after bleeding. Usually, a brain computerized tomography (CT) scan is performed, and bleeding is confirmed. Sometimes, bleeding may be so minuscule that a CT scan may not detect it. Lumbar puncture might be performed on these patients. If bloody cerebrospinal fluid is encountered, the diagnosis is confirmed. Below is a CT scan of a patient with subarachnoid hemorrhage (white areas in the brain).
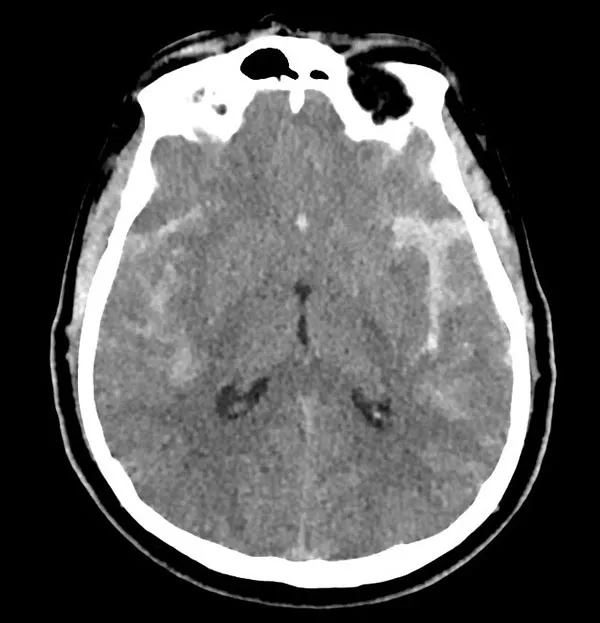
These clots may obstruct cerebrospinal fluid flow and cause acute hydrocephalus. Also, starting several days after hemorrhage, blood clots break down, releasing blood degradation products. This is a very dangerous time period since blood degradation products cause vasospasm – i.e., narrowing of brain arteries. The resultant effect is decreased flow to the brain with ischemic change, further aggravating the patient’s condition. In some cases, the hemorrhage may be very massive, and an aneurysm may rupture not only into subarachnoid space but also into the brain itself. Patients may have fallen into a coma and/or develop neurological deficits.
Aneurysms may cause compression of nearby cranial nerves. Second and third cranial nerves are usually very prone to this type of compression, and patients may experience blurry or double vision. Sometimes, aneurysms may be gigantic and cause brain compression, resulting in neurological deficits or epilepsy.
How is a brain aneurysm diagnosed?
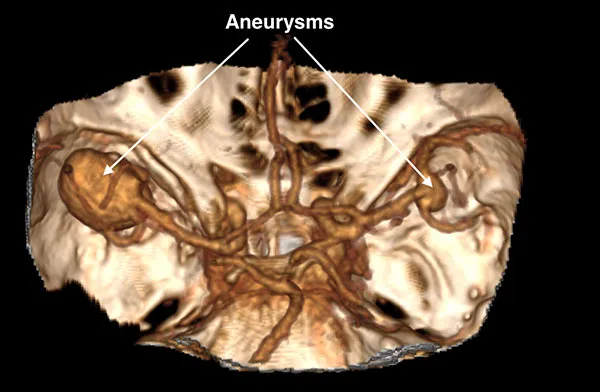
When a brain aneurysm is suspected, brain angiography (literally, vessel imaging) is required to demonstrate its presence, size, and location. Angiography may be performed on CT (CT angiography or CTA), MRI (MR angiography or MRA), or through catheters placed into brain vessels (Digital Subtraction Angiography). Although DSA is considered the gold standard for detecting brain aneurysms, it is an invasive procedure. CTA and MRA nowadays are capable of demonstrating the majority of aneurysms and avoiding DSA procedures. Below is the picture of the CTA of a patient who was referred for spontaneous subarachnoid hemorrhage and was found to have two aneurysms.
What is the treatment for brain aneurysms?
Treatment for aneurysms depends on their rupture status. If the aneurysm is found incidentally on a brain scan, usually, there is no need for urgent intervention. These cases are done electively. However, ruptured aneurysms should be treated as soon as possible to prevent re-bleeding.
There are two main treatment options for brain aneurysms – microsurgical clipping and endovascular treatment. Microsurgical clipping is performed by neurosurgeons and consists of approaching the aneurysm and placing a permanent clip across the neck of the aneurysm to obstruct the flow into it. This way, an aneurysm is effectively excluded from blood circulation. It is a very effective treatment modality.
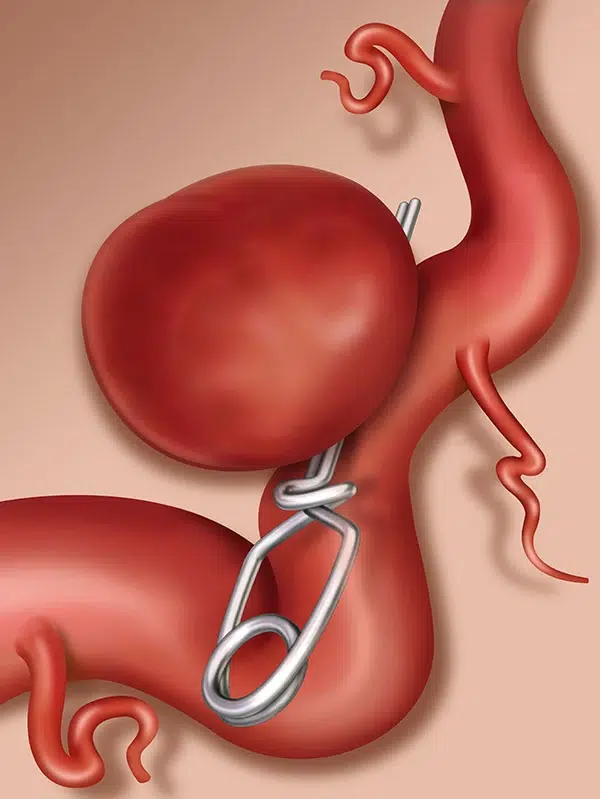
The rate of complete occlusion is high, and the recurrence following microsurgical clipping is very low. Another advantage of surgical intervention is the ability to remove blood clots from the brain and decrease the rate of vasospasm and hydrocephalus.
Endovascular treatment is a collective term that includes many various types of interventions that aim either to fill the aneurysm or to divert the flow from the aneurysm to reduce the chance of bleeding. These treatments are usually provided either by neurosurgeons or interventional radiologists. The major advantage is avoidance of open brain surgery, yet long-term occlusion rates are not as satisfactory as with microsurgical clipping. The decision to treat a particular aneurysm with surgery or endovascular means should be made by a specific, experienced team practicing both treatment modalities.
