What are the symptoms of the thoracic outlet syndrome?
Thoracic outlet syndrome symptoms depend on the type of TOS, but some of them are the same in different forms of the disease.
Neurogenic TOS – nTOS
Neurogenic TOS is caused by compression of the brachial plexus. Five cervical roots arising from the spinal cord – C5, C6, C7, C8, and T1 form a complex network of nerves in the shoulder called the brachial plexus. The brachial plexus is by far the most commonly affected structure in thoracic outlet syndrome, and this variant is called neurogenic or n-TOS. In the vast majority of cases, the lower part of the brachial plexus is affected. This section includes the C8 and T1 nerve roots, as well as the inferior trunk, which is formed by union of these two nerves. This lower section of the brachial plexus is in close contact with the first rib and first rib abnormalities and lead to compression of these nerves.
There are three main symptoms of n-TOS: pain, sensory and motor disturbances. Pain is by far the most common and enervating symptom. It is caused by mechanical compression or irritation of the brachial plexus. The pain is usually localized in the shoulder and can propagate to the head, neck, back, armpit, chest, arm, hand, fingers. The pain can be constant or intermittent. The pain is typically triggered by overhead activities such as haircare, phone holding etc.
Headache is one of the most common neurogenic TOS symptoms. 1 It usually starts at the base of the neck, spreads to the back of the head and then to the top of the head, and sometimes to the forehead and temples. Migraines are also common with thoracic outlet syndrome. Interestingly, surgery results in significant pain reduction and improved quality of life. 2 Facial pain is also very common in patients with TOS and well responds to surgical intervention. 3 Sometimes the pain is on one side of the neck and at the base of the head behind the ear or in the lower jaw. Patients may experience pain and dysfunction of the temporomandibular joint. In addition to headaches, patients may experience more concerning symptoms such as cognitive problems, lack of concentration, blurred vision, dizziness, chronic fatigue, ear pressure, tinnitus, sinus pressure, facial spasms, fainting, and facial flushing.

Chest pain is very typical of n-TOS. The pain can be quite severe and even resemble a heart attack, and patients may undergo diagnostic testing for cardiovascular disease. The pain usually worsens with physical activity, carrying groceries, and lifting the affected arm.
In most cases, the pain radiates from the shoulder to the arm, forearm and fingers. The ulnar side of the forearm, as well as the fourth and fifth fingers are usually affected. This part of the arm is innervated by the C8 and T1 nerve roots, which are most often affected in neurogenic TOS. The pain is usually accompanied by sensory disturbances such as tingling, burning, coldness, or numbness (hypesthesia) in the affected area. Physical activity triggers and worsens sensory symptoms. Overhead activities such as talking on the phone, combing hair, hanging curtains usually cause pain. Therefore, patients usually avoid these activities or change hands frequently during the task.

Occasional numbness is typical and is triggered by physical activity, such as carrying a bag. Some patients wake up numb and it may take several minutes for sensation to return. In some cases, patients may be unaware of the numbness due to severe pain and are surprised during neurological examination that pain and numbness actually coexist in the same area.
Sensory abnormalities may mimic ulnar or median nerve involvement and cause diagnostic challenges. Doctors may misdiagnose cubital and carpal tunnel syndrome instead of TOS, and patients may undergo unnecessary surgery.
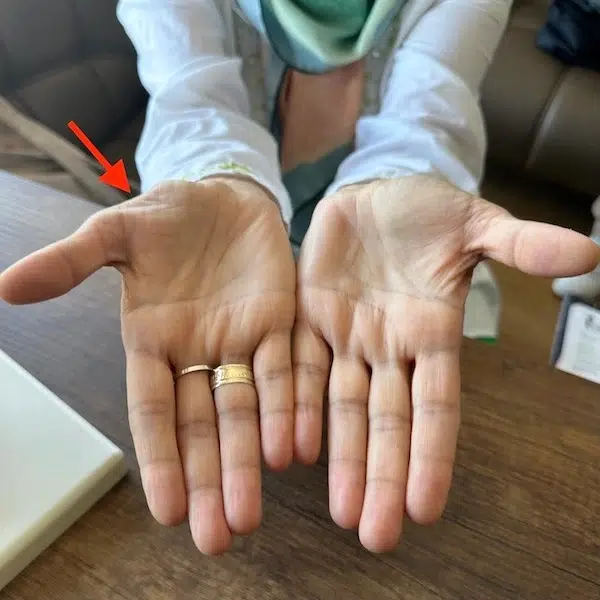
Motor deficits or muscle weakness are very common in TOS. Involvement of the hand muscles is typical, and patients experience symptoms of fatigue, clumsiness when performing small and precise movements, and weak grip of the hands (especially when opening a jar). These symptoms may later progress to significant weakness and atrophy (wasting) of the arm muscles (Gilliatt-Sumner hand).
Venous TOS – vTOS
Venous TOS – vTOS is less common than n-TOS. Subclavian vein compression is the cause of vTOS. This vein is the main drainage vessel carrying venous blood from the arm back to the heart. External compression causes narrowing and slows blood flow. As a result, the arm becomes filled with venous (dark blue, low oxygen) blood. Pain, cyanosis (blue discoloration) of the arm, hand, and fingers, swelling, and visible veins are typical symptoms of TOS. Symptoms may improve in lying position but quickly return when standing up. Swelling can be very significant and arm thickness maybe as much as twice of the normal arm.
The subclavian vein runs in the narrow space bordered by the first rib, subclavius muscle, costo-clavicular ligament and the anterior scalene muscle. This area is one of the critical location sites for subclavian vein on its way into the chest cavity. The area is pretty narrow to start with and becomes very narrow with arm abduction due to “nutcracker effect” of clavicle and first rib. In addition, hypertrophy of subclavius or anterior scalene muscle can worsen compression. Such hypertrophy is common among athletes and weightlifters causing intermittent subclavian blockage. McCleery syndrome is an occasional blockage of the subclavian vein following physical activity. 4 Rigorous physical work (especially overhead) causes significant compression of the subclavian vein to the degree of thrombosis, that is, a blood clot formation inside it, which leads to an almost complete blockage of blood flow. This form of v-TOS is called effort thrombosis or Paget-Schroetter disease. The clinical course may be further complicated if the clot breaks off and enters the bloodstream, causing pulmonary embolism (PTE). This condition is life-threatening and requires urgent intervention. Sudden chest pain, shortness of breath, and arrhythmia are symptoms of PTE. Chronic thrombosis of the subclavian vein leads to gradual narrowing. As a consequence, compensatory collateral veins dilate to bypass the blocked segment. Typically, some of these collateral veins are visible in the shoulder and upper chest areas.

Dialysis patients with therapeutic arteriovenous fistula are highly prone to developing vTOS. High blood velocity and turbulence can cause narrowing of the subclavian vein in the most vulnerable area, that is, between the clavicle and the first rib.
Pain is a common symptom of v-TOS. This may be due to venous congestion in the affected arm. It is usually proportional to the degree of congestion. The pain is usually accompanied by a tingling sensation in the hands and fingers and is triggered by physical activity. Muscle weakness may also be present. It should be noted that venous TOS is not as rare as is commonly believed. Although pure vTOS and its extreme variant, Paget-Shoretter disease, are quite rare, subclinical and less symptomatic vTOS quite often accompanies nTOS. Clinicians’ focus on neurological symptoms may miss symptoms of venous stasis and lead to unsatisfactory treatment outcomes.
Arterial TOS – aTOS
Arterial TOS – aTOS is the rarest form of TOS and is caused by compression of the subclavian artery. This artery is the main vessel supplying the arm, and blood flow decrease leads to limb ischemia (lack of oxygen). Ischemia may not be evident during resting when oxygen demand is low. However, exercise, physical activity, and working increase oxygen consumption by arm muscles, and ischemia emerges. Such excersize intolerance is called intermittent claudication. Cold exposure also decreases blood flow due to vasoconstriction, and this phenomenon is known as cold intolerance.
Pain, tingling, paleness, early fatigue, poikilothermia and coldness are presenting symptoms. In some cases, the subclavian artery may get thrombosed leading to sudden loss of blood flow to the arm. These acute cases require immediate intervention to avoid arm gangrene. Chronic thrombosis may narrow the artery (in addition to external compression) and induce intermittent ischemia. Thrombi may dislodge and travel along blood flow toward the arm and cause small ischemias, particulalry in the fingertips. ATOS cases are usually misdiagnosed as Raynaud syndrome. Occasionally aneurysms may develop at the site of subclavian artery compression. Aneurysm is a dilation of artery and is caused by weakening of its wall. Intermittent squashing of the artery damages and weakens its wall triggering aneurysm development. Endothelial (inner) linining may also get damaged leading to ulcerations and thrombus foramations. Therefore aneurysms (especially large ones) are frequently thrombosed. Sometimes thrombus might partially or fully occlude the subclavian artery leading to arm ischemia. If aneurysm is big enough it may show up as a soft pulsatile mass in the neck.

There is growing scientific evidence that thoracic outlet syndrome may impede brain’s blood supply. Such blood flow disruption is due to insufficient blood flow in the carotid and vertebral arteries which provide blood supply to the brain. Vertebal arteries branch off from the subclavian artery and any impairment of flow in the parent (subclavian) vessel may cause disturbance in the brach (vertebral), resulting in insufficient blood supply to the brain. Although the mechanism of vertebral (or vertebrobasilar) insufficiency is poorly understood, the permanent or temporary impairment of brain’s blood flow in TOS is well documented. In extreme cases, the patient may present with stroke due to significant brain blood flow. 5 However, in the vast majority of cases, symptoms are not so severe and tend to be intermittent. Exercise-induced symptoms are quite typical. Since vertebral arteries supply the brainstem, cerebellum, and back part of the brain, insufficient blood supply may result in disturbance of these brain regions. Symptoms may include dizziness, tinnitus, visual disturbances, and gait problems.
Recent scientific studies provide evidence that cerebral hyperperfusion (increased blood flow to head and brain) might be very common. Once the flow in subclavian artery is blocked, the blood is diverted toward the head causing cerebral hyperperfusion syndrome. 6 Contrary to common belief such increased flow is not very good for the brain and causes various symptons. The patients may experience headache, sense of pressure in the head, tinnitus, vertigo, pulsations and visual disturbances.
Combined symptoms
Vascular symptoms may be combined with neurogenic. In these cases, a combination of the above-mentioned symptoms may be present.
Next: Thoracic Outlet Syndrome Diagnosis
References
- Raskin NH, Howard MW, Ehrenfeld WK. Headache as the leading symptom of the thoracic outlet syndrome. Headache. 1985;25(4):208-210. https://doi.org/10.1111/j.1526-4610.1985.hed2504208.x[↩]
- Chahwala V, Tashiro J, Li X, Baqai A, Rey J, Robinson HR. Venous Thoracic Outlet Syndrome as a Cause of Intractable Migraines. Ann Vasc Surg. 2017;39:285 e285-285 e288. https://doi.org/10.1016/j.avsg.2016.05.109[↩]
- Zhang Z, Dellon AL. Facial pain and headache associated with brachial plexus compression in the thoracic inlet. Microsurgery. 2008;28(5):347-350. https://doi.org/10.1002/micr.20507[↩]
- McCleery R, Kesterson JE, Kirtley JA, Love RB. Subclavius and anterior scalene muscle compression as a cause of intermittent obstruction of the subclavian vein. Ann Surg. 1951;133(5):588-602 https://doi.org/10.1097/00000658-195105000-00002[↩]
- Palmer OP, Weaver FA. Bilateral cervical ribs causing cerebellar stroke and arterial thoracic outlet syndrome: a case report and review of the literature. Ann Vasc Surg. 2015;29(4):840 e841-844. https://doi.org/10.1016/j.avsg.2014.12.008[↩]
- Larsen K, Galluccio FC, Chand SK. Does thoracic outlet syndrome cause cerebrovascular hyperperfusion? Diagnostic markers for occult craniovascular congestion. Anaesthesia, Pain & Intensive Care. 2020;24(1):69-86 https://doi.org/10.35975/apic.v24i1.1230[↩]
