What is Thoracic Outlet Syndrome: The Definition
Thoracic outlet syndrome, or simply TOS, is a general term that describes several conditions associated with the compression of nerves and/or blood vessels in the thoracic outlet area, which represents the upper exit (outlet) of the chest cavity.
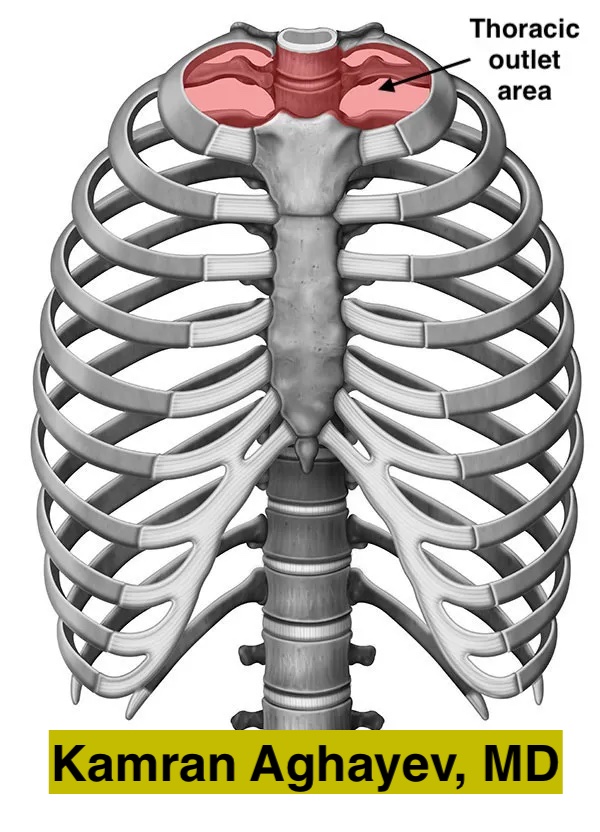
What is the thoracic outlet area?
The thoracic outlet is a heart-shaped area located at the top of the chest cavity. Structurally, this area is bounded by the first thoracic vertebra, the left and right first ribs, and the sternum. It contains important organs and, therefore, has great clinical significance.
What structures are affected by Thoracic Outlet Syndrome?
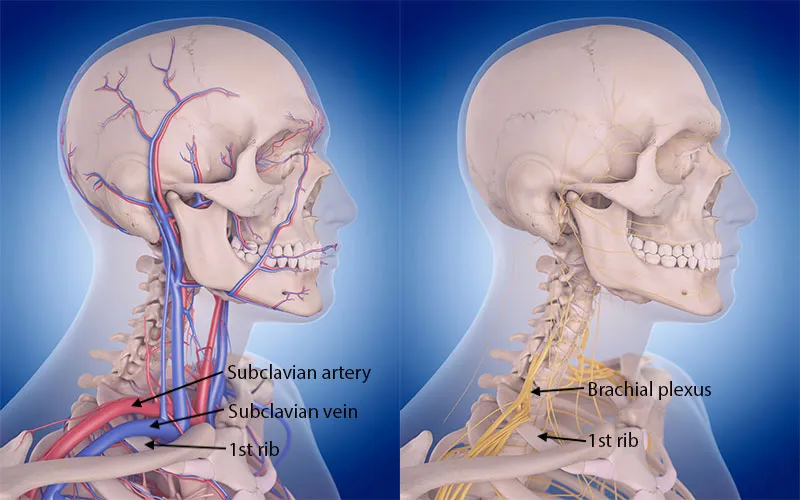
The neurovascular bundle is pressed in thoracic outlet syndrome. In summary, this bundle includes the brachial plexus, the subclavian artery, and the vein.
Brachial plexus
Five nerves coming off the spinal cord (C5, C6, C7, C8, and T1) form a complex network called the brachial plexus. Consequently, the brachial plexus branches off several nerves that travel to the neck, shoulder, upper chest, and arm. These nerves carry impulses between the spinal cord and the arm. They control every aspect of arm and shoulder function: skin sensation, muscle movements, sweating, the tone of blood vessels, etc.
Subclavian vessels
The subclavian artery and vein are the main vessels providing blood flow to and from the arm. They pass above the first rib alongside the brachial plexus on their route to the arm.
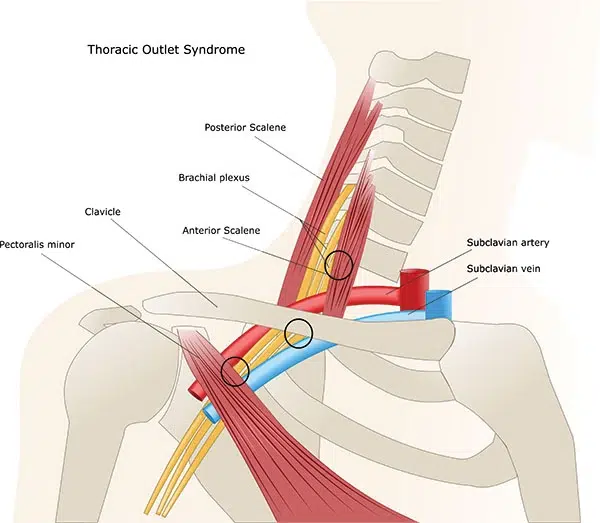
Anatomical relationships in the thoracic outlet area
The nerves and blood vessels travel directly above the first rib, which has two specific grooves to fit the subclavian artery and vein. Additionally, C8 and T1 nerve roots and the lower trunk of the brachial plexus also directly touch the first rib. The brachial plexus and subclavian artery pass through a narrow anatomical window called the scalene triangle. This triangle has three borders – two scalene muscles (anterior and middle) and the first rib. The subclavian vein, on the other hand, passes through the costoclavicular or venous triangle. Subclavius muscle, anterior scalene muscle, and the first rib form the venous triangle. The subclavius muscle may smash the vein against the first rib.
Types of Thoracic Outlet Syndrome
There are three clinical TOS forms:
- Neurogenic TOS – nTOS. The most common form—approximately 80-85% of cases. Compression affects the brachial plexus, and symptoms develop due to neural compression.
- Venous TOS – vTOS. Far less common – about 10-15% of cases. Compression affects the subclavian vein, and symptoms develop due to insufficient blood return from the arm.
- Arterial TOS – aTOS. The least common form—approximately 1-2% of all cases. Compression affects the subclavian artery, and the symptoms develop due to insufficient flow to the affected arm.
Causes of thoracic outlet syndrome
Thoracic outlet syndrome is a term that describes the site (location) of the disease rather than the cause. This term is similar to other entrapment neuropathies, for example, carpal tunnel syndrome. Generally, it is customary in peripheral nerve surgery to classify the conditions according to the pathology site. However, the term doesn’t contain information about the cause of the problem. Occasionally, the compressing factor can be obvious (like a cervical accessory rib or a tumor) in imaging studies. Unfortunately, this is not the case for the majority of patients, even with advanced imaging.
There are several conditions predisposing to thoracic outlet syndrome. Women are affected 3-4 more often than men. Sometimes, people who work with repetitive arm and hand movements develop TOS. Poor posture, particularly shoulder slouching, can cause compression. Various congenital and acquired conditions responsible for TOS development are summarized below:
Cervical accessory rib
The normal human body has 12 pairs of ribs, forming the chest cavity. Occasionally, people may have accessory or extra cervical ribs. Recently, a large literature review has found that approximately 1.1% of the population has cervical ribs. 1 Furthermore, the occurrence of accessory cervical ribs in people with thoracic outlet syndrome is 29% – approximately 25 times more than in the general population. 2
The shape and size of the rib may vary dramatically—from a slightly longer C7 transverse process to an almost normally looking rib. If the extra rib is big, its tip usually touches the first rib. X-rays explicitly show cervical additional ribs, yet unexperienced eyes may fail to recognize them.

Genetic causes of anomalous cervical ribs
Unfortunately, the exact mechanism responsible for additional cervical rib formation is unknown, but there is evidence that it might be due to a glitch in HOX genes. HOX genes or homeobox genes are responsible for the sequence of events responsible for correct body segmentation. Disturbances and mutations affecting these genes lead to a number of vertebral anomalies and cervical ribs. Studies showed that mice with mutant HOX genes develop additional ribs at the seventh cervical vertebra. 3 Interestingly, HOX genes also play a certain role in cancer development, and there is evidence that the occurrence of additional ribs is higher in cancer patients, further supporting the HOX hypothesis. 4
First rib abnormalities
The first rib is a curved flat bone lying between the first thoracic vertebra and sternum. Anomalous, broken, or misplaced first ribs can cause TOS by stretching or compressing the neuro-vascular bundle. Congenital abnormalities such as fused ribs or bifid ribs are well-known causes of TOS. One study found that thick first ribs may cause TOS. 5 Another study found that abnormal bone prominence near the sternal end of the first rib is responsible for venous TOS development. 6
Trauma is also a significant contributor to TOS. Fractured first ribs may not heal appropriately. As a result, the fracture site may develop either excessive bone callus formation or pseudoarthrosis (lack of bone healing leading to tumor-like swelling). These inappropriately healed first ribs can also cause thoracic outlet syndrome. Tumors of the first rib, including benign lesions like hemangiomas, expand the bone and compress the nearby neuro-vascular bundle.
Plain X-rays can diagnose first rib abnormalities, as in the case of cervical ribs. However, the complex anatomy of the first rib, overlapping nearby bones, and variety of first rib pathologies make thoracic outlet syndrome diagnosis difficult for an untrained eye. Therefore, only experts with vast experience can correctly pinpoint first rib abnormalities on X-rays. CT scan with 3D reconstruction can visualize first ribs much better than X-rays and is a superb imaging modality when it comes to bone abnormalities.
Fibromuscular soft tissue bands
Fibromuscular soft tissue bands constitute a significant portion of TOS cases. Occasionally, the cause of compression may be an abnormal muscle, a fibrous band, or a combination of them. For example, abnormal muscle like scalenus anticus, scalenus minimus and subclavius posticus can cause neuro-vacsular compression yet they are relatively rare. These bands of fibro-muscular tissue run from various portions of the spine (usually from the C7 transverse process) to the first rib stretching and compressing the neuro-vascular bundle. 7
Hypertrophic muscles
Hypertrophic muscles also may cause neurovascular compression. People using their arms and hands extensively for work and sports are especially prone to this type of TOS. Naturally, athletes frequently develop TOS. Scalene muscle hypertrophy usually results in n- and a-TOS (since both the artery and brachial plexus run inside the scalene triangle). 8 Sublclavius muscle hypertrophy, on the other hand, may cause compression and even thrombosis of the subclavian vein (Paget–Schroetter disease).
Costo-clavicular compression
Both the clavicle and first rib make a joint with the upper part of the sternum. The first rib has little mobility, whereas the clavicle is a very mobile bone. The clavicle makes another joint with the scapula. It is basically a lever between the fixed sternum and the mobile scapula. Normally, the gap between the clavicle bone and the first rib – costo-clavicular space is quite wide. The neuro-vascular bundle passes through this gap just above the first rib and below the clavicle. However, with arm abduction, the costo-clavicular gap may become very narrow due to the movement of the scapula. This effect is called the “nutcracker mechanism” and may narrow costo-clavicular space. Studies show that in normal people, the gap remains wide enough that there is no pressure on nerves or blood vessels. In TOS patients, the gap may become critically narrow, resulting in neuro-vascular compression. 9

Blood vessels
Occasionally, blood vessels branching from subclavian vessels may loop around the brachial plexus and cause compression. These small vessel causes are very difficult to diagnose radiologically and are usually discovered during surgery. 10
Chronic kidney disease and dialysis
Arterio-venous fistula provides easy vascular access in hemodialysis patients. However, the major problem is increased blood flow and turbulence in the subclavian vein. This leads to central venous narrowing, and the thoracic outlet area is a particularly vulnerable region. Like in most vTOS cases, such stenosis usually develops in the costo-clavicular (or venous) triangle due to the “nutcracker effect” between the clavicle and the first rib. 11
Next: Thoracic Outlet Syndrome Signs and Symptoms
Explore the next chapter to learn about the various symptoms of Thoracic Outlet Syndrome (TOS), including numbness, neck pain, shoulder pain, and muscle weakness. Discover how these symptoms, which affect the upper chest, arms, and nerves, can manifest as headaches, dizziness, and other sensory disturbances in different types of TOS.
See Also: Thoracic Outlet Syndrome Treatment
Explore this section to understand the various treatment options for Thoracic Outlet Syndrome (TOS), including thoracic outlet decompression surgery and physical therapy. Learn how surgical treatment aims to alleviate TOS symptoms by addressing the underlying causes, while also considering potential complications and the role of nerves and blood vessels in the condition.
References
- Henry BM, Vikse J, Sanna B, et al. Cervical Rib Prevalence and its Association with Thoracic Outlet Syndrome: A Meta-Analysis of 141 Studies with Surgical Considerations. World Neurosurg. 2018;110:e965-e978. https://doi.org/10.1016/j.wneu.2017.11.148[↩]
- Henry BM, Vikse J, Sanna B, et al. Cervical Rib Prevalence and its Association with Thoracic Outlet Syndrome: A Meta-Analysis of 141 Studies with Surgical Considerations. World Neurosurg. 2018;110:e965-e978. https://doi.org/10.1016/j.wneu.2017.11.148[↩]
- Horan GS, Wu K, Wolgemuth DJ, Behringer RR. Homeotic transformation of cervical vertebrae in Hoxa-4 mutant mice. Proc Natl Acad Sci U S A. 1994;91(26):12644-12648. https://doi.org/10.1073/pnas.91.26.12644[↩]
- Merks JH, Smets AM, Van Rijn RR, et al. Prevalence of rib anomalies in normal Caucasian children and childhood cancer patients. Eur J Med Genet. 2005;48(2):113-129. https://doi.org/10.1016/j.ejmg.2005.01.029[↩]
- Chang CS, Chuang DC, Chin SC, Chang CJ. An investigation of the relationship between thoracic outlet syndrome and the dimensions of the first rib and clavicle. J Plast Reconstr Aesthet Surg. 2011;64(8):1000-1006 https://doi.org/10.1016/j.bjps.2011.03.017[↩]
- Gharagozloo F, Meyer M, Tempesta B, Strother E, Margolis M, Neville R. Proposed pathogenesis of Paget-Schroetter disease: impingement of the subclavian vein by a congenitally malformed bony tubercle on the first rib. J Clin Pathol. 2012;65(3):262-266 https://dx.doi.org/10.1136/jclinpath-2011-200479[↩]
- Roos DB. Congenital anomalies associated with thoracic outlet syndrome. Anatomy, symptoms, diagnosis, and treatment. Am J Surg. 1976;132(6):771-778. https://doi.org/10.1016/0002-9610(76)90456-6[↩]
- Qaja E, Honari S, Rhee R. Arterial thoracic outlet syndrome secondary to hypertrophy of the anterior scalene muscle. J Surg Case Rep. 2017;2017(8):rjx158. https://doi.org/10.1093/jscr/rjx158[↩]
- Illig KA, Doyle AJ. A comprehensive review of Paget-Schroetter syndrome. J Vasc Surg. 2010;51(6):1538-1547. https://doi.org/10.1016/j.jvs.2009.12.022[↩]
- Hanna A, Bodden LO, Siebiger GRL. Neurogenic Thoracic Outlet Syndrome Caused by Vascular Compression of the Brachial Plexus: A Report of Two Cases. J Brachial Plex Peripher Nerve Inj. 2018;13(1):e1-e3. https://doi.org/10.1055/s-0037-1607977[↩]
- Davies MG, Hart JP. Venous thoracic outlet syndrome and hemodialysis. Front Surg. 2023;10:1149644. https://doi.org/10.3389/fsurg.2023.1149644[↩]
