What is the trigeminal neuralgia?
Trigeminal neuralgia (TN, tic douloureux) is a disease characterized by pain in the distribution of the trigeminal nerve in the face.
How does the trigeminal neuralgia develop?
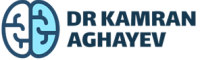
The trigeminal nerve is the only nerve providing sensory innervation to the human face. Sensory signals from the skin, like warm/cold, touch, pressure, vibration, and pain, reach the brain via this nerve. The trigeminal nerve sprouts out to three main divisions, which destinate the forehead, cheek, and jaw. These three branches unite into a single nerve, which enters the brainstem after passing a short distance in the subarachnoid space.
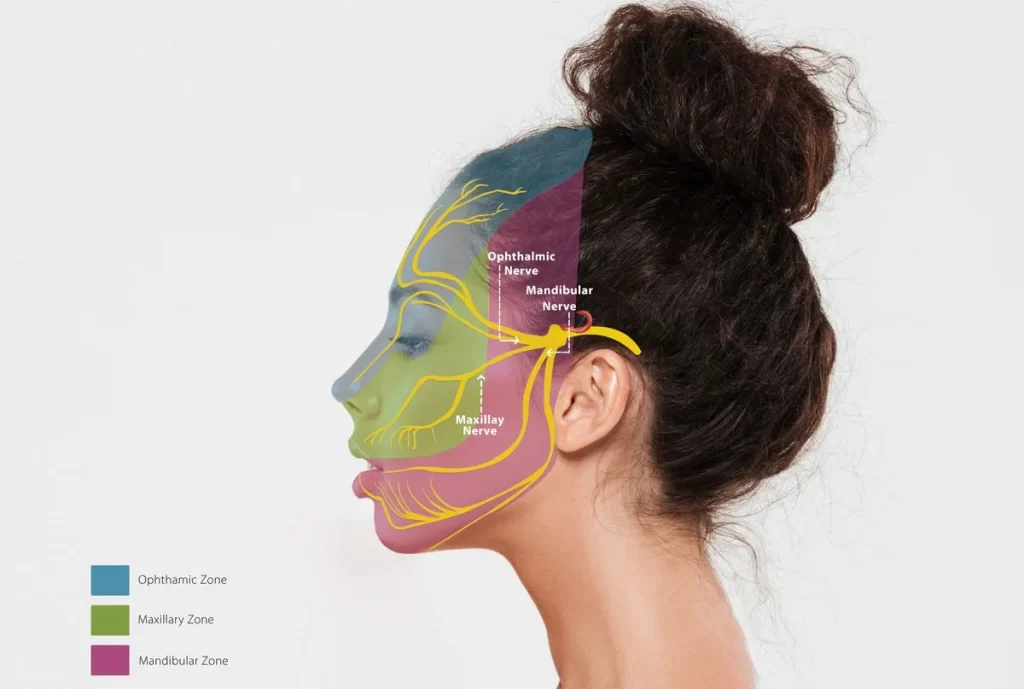
This space is the passing location for nerves entering and exiting from the brain as well as arteries and veins providing blood flow to and from the brain. Sometimes, a nearby artery or vein may wrap around the nerve and compress it. Since the pressure inside the artery and vein is not constant and changes with heartbeats, the pressure is pulsatile in nature. Therefore, individual nerve fibers suffer and get irritated, resulting in trigeminal neuralgia.
What are the symptoms of trigeminal neuralgia?
Typically, TN is manifested by sudden, intensive, excruciating, sharp, electric, or thunder-like painful attacks lasting a few seconds (tic douloureux). These painful bursts can be precipitated by speaking, laughing, touching, eating, tooth brushing, i.e., anything stimulating the trigeminal nerve. This form of the disease is called typical trigeminal neuralgia or type 1 (TN1).
On the contrary, type 2 (TN2), or atypical form, is characterized by long-lasting dull pain. One patient may experience both pain types alternatively or superimposed on each other. Usually, there is an associated numbness in the affected area, but the patients may be unaware of this due to pain.
Usually, the pain is exhibited in one of the branches of the trigeminal nerve. Sometimes, two or all three branches may be affected. The mandibular branch providing innervation to the jaw and lower teeth are most frequently affected. Maxillary branches, providing sensation to the cheek and upper teeth, are less commonly affected. The ophthalmic branch, innervating the forehead, is the least affected nerve.
How is the diagnosis of trigeminal neuralgia made?
The diagnosis of trigeminal neuralgia is based on clinical presentation. Physical examination is unremarkable but may show hypoesthesia in the distribution of one or more trigeminal nerve divisions.
Currently, there are no laboratory or imaging modalities to confirm the diagnosis. In the vast majority of cases, the symptoms are very typical, and the diagnosis is straightforward. However, in other cases, the patients may exhibit confusing pain patterns, leading to misdiagnosis and mistreatment. This is especially true for cases presenting with tooth pain. These patients may undergo unnecessary tooth treatment and even extraction.
Although the radiological diagnosis of trigeminal neuralgia is not an available demonstration of vascular compression, it is possible with a fine, thin-sliced FIESTA or CISS sequence MRI scan. However, one should remember that vascular compression is not always symptomatic and should be correlated with clinical findings for an accurate diagnosis. In some cases, the compressing factor may be a tumor or a benign arachnoid cyst.
What is the treatment of trigeminal neuralgia?
The initial treatment of trigeminal neuralgia is medical. Carbamazepine is the drug of choice and provides pain relief in the majority of cases. Other medications like gabapentin or topiramate may also be helpful in selected cases. The patient should bear in mind that medical treatment does not provide a cure and is aimed at interfering with the propagation of abnormal signals within the nerve. Therefore, these medications are taken lifelong.
Cases refractory to medical treatment, i.e., not responding to conservative treatment, should be managed surgically. In some cases, the disease is progressive, i.e., after initial success with mediation, the pain recurs later on. If the compressing factor is a tumor or a cyst, the condition is treated with surgical intervention.
Trigeminal neuralgia surgery
The surgical treatment of choice is microvascular decompression (MVD). This procedure is aimed to permanently relieve the pressure from the nerve by separating the blood vessels. Usually, a tiny Teflon paddy is inserted in between them to keep the two structures apart and provide lasting relief for the nerve.
Microvascular decompression of the trigeminal nerve: how the surgery is performed
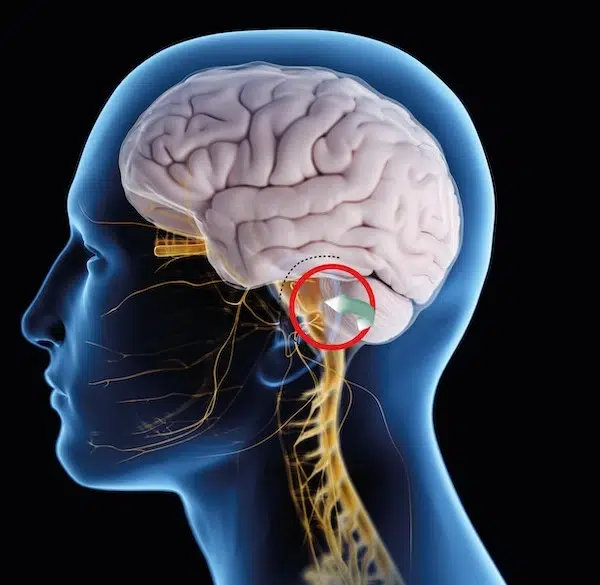
The microvascular decompression procedure is performed under general anesthesia. A small opening in the skull called craniotomy is performed behind the ear. Then, the surgeon works around the cerebellum to find the trigeminal nerve.
The affected nerve is exposed and separated from the compressing artery and/or vein. A Teflon sponge is inserted and left permanently.
The patients can usually leave the hospital in 1-2 days. Microvascular decompression has a high success rate and is considered the best surgical treatment modality for trigeminal neuralgia.